Below are summaries of some of the many systemic actions we have been involved in over the past 5 years. On the side menu, you will see our most recent/ongoing systemic projects, partnerships and involvements.
If you have any questions about Systemic Advocacy in the Health System, or about any of our listed involvements, please email info@hconc.org.au

Background
In 2015, the Health Consumers’ Council was funded to co-ordinate a project to build on the recommendations from the November 2014 Forum, Improving Consumer Involvement in the Alcohol and Other Drug Sector. An Alcohol and Other Drug Advisory Group (AODAG) comprising government agencies, not for profit organisations and consumers was set up to oversee progress.
The project specifically addressed the following two recommendations:
- to develop a common set of principles for engagement
- outline best practice engagement strategies for the sector
In 2017 the WA Primary Health Alliance funded HCC to support the ongoing work of the Alcohol and Other Drug Advisory Group (AODAG) to oversee a new project entitled “Improving Consumer Involvement in the Alcohol and Other Drug Sector”.
It was agreed that the term ‘alcohol and other drug consumers’ was inclusive of current users, service users, potential service users, family members and supporters.
The Alcohol and Other Drug Consumer & Community Coalition (AODCCC) was incorporated in June 2018 in response to the need and support for an AOD specific consumer advocacy body. We have recently received funding from the Mental Health Commission in order to progress our establishment and have now released our Mission, Vision and Values.
AODCCC Membership
Membership is open to people who use or who have used alcohol and other drugs, their family members and significant others. A link to an online membership application can be found here and on the Facebook page. Hard copy applications are available here and can be emailed to info@aodccc.org.
Management Committee
Full details of the current Management Committee are provided on the Australian Charities and Not-for-profit Commission (ACNC) website.
Contact AODCCC
For any information please contact:
Email info@aodccc.org
Phone (08) 6311 8402
Cancer Care
The Cancer Plan was released in February 2020 setting out the next five years of strategy in relation to cancer services. This work was undertaken by the WA Department of Health, and the Health Consumers’ Council supported the project through running a community survey and developing consumer videos reflecting consumer patient journey experiences. A summary of survey results is available here. The launch event featured a moving and articulate presentation from Advisory Group member Susannah Morris, who ensured the consumer voice was at the heart of the plan as much as possible.
Cancer Research
In May 2019 the Health Department’s Health Research Future Fund sought feedback on the involvement of consumers in cancer research. A large forum was convened with researchers and clinicians across the sector. HCC was funded to enhance the consumer voice into the process. We undertook a consumer survey, and presented a short video with consumer and carer experiences of being involved in research. Click the link for the Consumer insights in Medical Research Cancer PowerPoint.
In summary, we strongly agree with the National Health and Medical Research Council that:
“Consumer and community involvement is about research being carried out with or by consumers and community members rather than to, about or for them.”
The Cost of Cancer Care
The Health Consumers’ Council partnered with Cancer Council WA to find out whether people are making informed financial decisions about where to get their cancer care.
We developed a short survey to find out more about the issue, and a report of the findings is here.
Dental Care
Access and costs are two issues we hear about frequently from consumers when it comes to dental care.
We have previously held a seat on the State Oral Health Advisory Committee; spoken on the radio with Geoff Hutchison about a consumer’s costs related to a child’s wisdom teeth; and run a survey to gather consumer stories and views on dental health. In 2023 we promoted a survey to encourage consumers to share their experiences as part of the Senate Select Committee into the Provision of and Access to Dental Services in Australia.
Digital Health
Our work in the digital health space is ongoing. Below is an archive of some of the previous work we have been involved.
There is so much going on in the digital health space. It is a complex area and difficult to know what issues need to focus on. People are rightly concerned about their data and its privacy. But being able to share your health information quickly could mean the difference between life and death. Queensland Health developed a Consumer Charter on Digital Health which aims to reflect consumer priorities and needs in relation to digital health.
In WA the Digital Health Strategy 2020-2030 was released, and a key initial deliverable will be creating a statewide electronic medical record in our hospitals. This may seem confusing, given that the My Health Record was implemented nationwide in 2019. As at December 2019, 22.68 million Australians had a My Health Record, with 2.4 million of those in WA. (See here) A key thing to remember is that:
- An electronic health record is designed to have a more overall view of someone’s health, across hospitals, GPs, pharmacists etc.
- A medical health record tracks medical care usually within one hospital.
We are currently working with the WA Department of Health to develop a Consumer Charter which focuses on digital health. HCC are convening 10 Kitchen Table Discussions on the topic and is currently seeking Discussion Hosts. The Kitchen Table Discussion comments will be used to form a Consumer Charter – this will include non-negotiable principles to guide future direction.
My Health Record Resources
In 2019, the Australian Digital Health Agency released a number of new resources, and we partnered with them to share them on our website and through social media. We also undertook a Consumer Survey – you can find the full report of our work here.
If you are using My Health Record, we recommenced you log in to take a look at your information and update your privacy settings. These brochures provide further information on how to use your My Health Record now that it has been set up.
- Your Health Information securely in one place (general information on how your health records are stored)
- Control who can look at your health information (includes how to set privacy controls)
- How is your health information protected (more information on privacy and security)
How can I find out more?
Check out these Frequently Asked Questions
Please email us if you have any concerns regarding the My Health Record and we will ensure you are given access to the information you need.
- Empowering Health Consumers with Disabilities – Resource List
- WA Getting Ready to Go Home (NDS project to improve the transition experience for people with a disability from hospital to community)
HCC partnered with People With disabilities WA to deliver a project which examined health literacy materials and put them to the test of disability friendliness. The project delivered nine training sessions on Disability Health Rights for people with disabilities, and their carers, family and support people. Topics covered included: rights, ideas for getting better care, where to go for help, medical records and information sharing, and navigating the health system.
A series of booklets and videos were produced for this project, and are linked below. Working group members also shared their views on how health services could engage more with people with disabilities at this blog article:
Plain English
- Better Healthcare for People with Disabilities – PE
- Better Hospital Care for People with Disabilities – PE
Easy-read
- Better Healthcare for People with Disabilities – ER
- Better Hospital Care for People with Disabilities – ER
Plain-text (screen-reader compatible)
- Better Healthcare for People with Disabilities – PT
- Better Hospital Care for People with Disabilities – PT
Videos
In 2020, Health Consumers’ Council (HCC) worked with the Patient Safety Surveillance Unit in the Department of Health to learn more about how consumer feedback – including complaints and compliments – is collected, provided, and used for improving health services. We held a number of workshops with consumers and we also held telephone interviews with some consumers in regional areas. We held targeted sessions for Aboriginal community members, and Consumers of Mental Health WA ran a targeted session for consumer of mental health services.
Click to see issues, barriers and ideals from this consultation
Care Opinion
In 2020 the Patient Opinion platform, an independent, moderated place for people to provide feedback, was renamed to Care Opinion. This platform is now one portal for people to provide feedback on health and social services. It mirrors the same platform available in the UK, which uses the power of story to transform health and human services.
A non-profit organisation moderates the platform, and services subscribe to be able to receive notifications, reports etc. WA is the first state to have every public hospital as a subscriber. You can find out more or post a story here.
WA Health Complaint Policy Review
The Department of Health (DoH) consulted on a revised version of the WA Complaints Management Policy and these new versions appear below. We undertook a series of consultations to support the work survey and have collated this feedback.
- Updated Complaints Management Policy – main draft policy – this is mandatory for WA Health services
- Updated Complaints Management Guideline – supporting document to expand on how the implementation of the policy – non-mandatory
- Updated Complaints Management Toolkit – supporting document including suggested templates for letters and forms – non-mandatory
WA Health Review of the complaints and feedback process
Following on from this consultation and the release of the new complaints guidelines, DoH consulted about the process of making a complaint and giving feedback. We heard about the many barriers to giving feedback, including concerns about what might happen to the feedback. This was especially prominent in the discussions we had with Aboriginal people. It was also raised that there is no easy way to give feedback about the whole system, not just one health service.
 Informing New Models of Primary Care was a 6 month collaborative project between the WA Primary Health Network (WAPHA), Health Consumers’ Council, and Curtin University undertaken in 2017. Primary Care refers to the care you receive from your GP and other health care providers outside of the hospital system. WAPHA is supported by funding from the Australian Government under the nation’s Primary Health Network Program.
Informing New Models of Primary Care was a 6 month collaborative project between the WA Primary Health Network (WAPHA), Health Consumers’ Council, and Curtin University undertaken in 2017. Primary Care refers to the care you receive from your GP and other health care providers outside of the hospital system. WAPHA is supported by funding from the Australian Government under the nation’s Primary Health Network Program.
Prior to this project being established, WAPHA and Curtin undertook consultations with general practice staff to inform how care can best be provided to people to keep them well and out of hospital as much as possible.
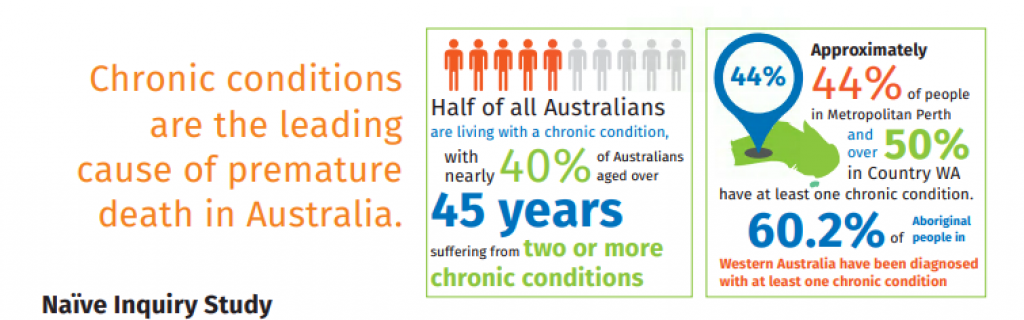
Informing New Models of Primary Care project was the second stage, and HCC worked with WAPHA and Curtin but this time focusing on the experience of people who access GP services. It involved convening a series of focus groups with people with multiple chronic health conditions with management under a Care Plan. Findings of these discussions have been compiled in the Naive Inquiry Brochure and were shared with the community at a community forum held on 1st December 2017. This forum provided an opportunity to further the conversation on the developing models of care.
Have you seen the Netflix Documentary The Bleeding Edge? In not, watch it now…
The day before the National Mesh Forum, which was convened on 5th April 2019 by the Health Consumers Councils across Australia and funded by state health departments, the Therapeutic Goods Administration (TGA) released Action Plan for Medical Devices. This was discussed at the Forum and is the culmination of some months work, but health consumers councils were not included in its development.
Strategies on the Plan:
Strategy 1
Improve how new devices get on the market
Strategy 2
Strengthen monitoring and follow-up of devices already in use
Strategy 3
Provide more information to patients about the devices they use
If there’s one thing consumers need to know…
Devices do not need to have as much evidence behind them as medications in order to be listed with the TGA. This is in part reflects the assumption that there is a detailed consent conversation between patients and their surgeons. We would urge all people to think of any procedure requiring any implanted medical device as an experimental treatment, and consent with that level of attention and care.
In essence, medical device companies assure TGA of the safety of their devices. It is a highly competitive and lucrative market, every bit as powerful as pharma, or perhaps more so. Post-market testing is supposed to occur, noting when complications occur and ensuring the TGA are aware. This doesn’t happen as much as it needs to, and is not compulsory for surgeons, although it is for medical device companies. Technically the TGA can prosecute medical device companies who don’t advise of complications but in practice this happens rarely.
Again, we recommend you watch the Bleeding Edge Documentary to understand more and what’s at stake for patient safety.
Bleeding Edge Documentary
America has the most technologically advanced health care system in the world, yet medical interventions have become the third leading cause of death, and the overwhelming majority of high-risk implanted devices never require a single clinical trial.
In The Bleeding Edge, Academy Award nominated filmmakers Kirby Dick and Amy Ziering (The Invisible War, The Hunting Ground) turn their sights on the $400 billion medical device industry, examining lax regulations, corporate cover-ups, and profit driven incentives that put patients at risk daily.
Across the globe there is an investigation underway by the International Consortium of Investigative Journalists about how medical devices are listed on the different jurisdiction’s list of approved devices. Called The Implant Files, the Consortium’s website provides latest news and updates in relation to implants.
The Health Consumers’ Council in WA recently noted the implications for how devices are put onto our Therapeutic Goods Administration (TGA) list through the work done on the Pelvic Mesh Inquiry held in 2017-18. In summary, the TGA often relies on slim evidence from other jurisdictions to approve a device, and whether there are any reports of post implant complications to confirm a device’s safety. However, reporting complications is not compulsory, and very often, clinicians don’t. They may not be aware that there is a trend, thinking “it’s only this one person, so is it relevant?” or for whatever reason, they don’t report. Consumers can report faults in implants they have had put into their body, if they know there is a place to do so on the TGA website, and if they know the serial number of the device. In other words, this is also not likely.
There is no easy way of knowing which human being has which implant, as there are only registers for certain kinds of devices, and records are often not digitised or easily shareable for it to be easy to do a product recall. It should be like doing an airbag recall for your car, but it isn’t.
The Health Issues Centre in Victoria has begun an anonymous survey for consumers who think they may have been impacted by implants, which you can complete by clicking on this link. Hernia mesh has already emerged as one of the leading implants causing pain and suffering for patients.
A GLOBAL HEALTH CRISIS – PELVIC MESH IMPLANTS
It has taken some time for the scale and extent of the impact of pelvic mesh implants for women to treat stress urinary incontinence and pelvic organ prolapse. Once hailed as the perfect solution for an enduring surgical fix for these non-life-threatening conditions, it has left a swathe of women with permanent, life altering consequences. Persistent pelvic pain at rest. Inability to have sex. Inability to continue working, and the financial impact often amplified by failed marriages as the lack of intimacy took its toll. The full list of complications is listed on the Therapeutic Goods Administration mesh hub.
In 2017 Australia undertook a Senate Inquiry – entitled Number of women in Australia who have had transvaginal mesh implants and related matters. We literally did not know how many women had been impacted. There were 13 recommendations in the final report, with a mix of federal and state responsibilities to effect implementation. There was even one on effective informed consent processes. It was clear from submissions and hearings that women were not informed about the potential horrific consequences of their choice, and that the mesh is extremely complex to remove. With the divide of responsibility between state and federal governments and the fact that most of the implant surgeries were performed in private hospitals, it is difficult to track real progress. Some meshes have been banned from use, but by no means all. Many women are still unaware that their sequelae of symptoms are related to their mesh implants. GPs and specialists may also be unaware.
WA PELVIC MESH SUPPORT GROUP
The peer support group the WA Pelvic Mesh Support Group has its own website and is an essential stakeholder in WA’s response to the mesh crisis.
WA PELVIC MESH COMPLICATIONS CLINIC
This clinic has been set up in King Edward Memorial Hospital and has been operating since 2017. There is a committee of clinicians and consumers who meet to discuss the clinic’s model and progress, as this area is complex and changing. The committee continues to aim to advance the recommendations of the Inquiry.
UNFINISHED BUSINESS – A NATIONAL FORUM ON THE IMPACT OF MESH IMPLANTS
 A National Mesh Implant Forum was held in Melbourne on Friday April 5, 2019, to consider all aspects of Australia’s mesh implant crisis. The Forum was proudly convened by the Health Issues Centre and Health Consumers NSW, Health Consumers Queensland, Health Consumers’ Council (WA), Health Consumers Alliance of South Australia, Health Care Consumers (ACT), Health Consumers Tasmania.
A National Mesh Implant Forum was held in Melbourne on Friday April 5, 2019, to consider all aspects of Australia’s mesh implant crisis. The Forum was proudly convened by the Health Issues Centre and Health Consumers NSW, Health Consumers Queensland, Health Consumers’ Council (WA), Health Consumers Alliance of South Australia, Health Care Consumers (ACT), Health Consumers Tasmania.
The event brought together mesh injured consumers, carers, regulatory authorities, health officials, the Chair of the Senate Inquiry into mesh and consumer advocates to create solutions and bring about real change. The forum considered not only the impact of pelvic mesh, but the emerging parallel crisis involving people who have received hernia mesh implants. A full report is available here.
NEW REPORT – HERNIA MESH IMPLANTS – CONSUMER SURVEY
Health Issues Centre Victoria initiated the Mesh Device and Implant Failure study late last year and of the respondents, a sizeable 183 patients have already reported major problems with their hernia mesh implants. 70 per cent of these are men. You can read the report here.
According to publicly available figures nearly 100,000 Australians are hospitalised for hernia each year. However, the numbers of patients that go on to have pelvic mesh implants and that are negatively impacted is not known. People who would like to report complications of hernia procedures using mesh can complete the survey here.
PELVIC MESH FAQs
What is pelvic mesh?Pelvic Mesh refers to polypropylene mesh implants to treat women treated for stress urinary incontinence or pelvic organ prolapse.
What are the complications of pelvic mesh?Complications include pain, inflammatary reactions to the mesh, persistent infections, bleeding, with the mesh kinking, moving or migrating and causing damage to surrounding organs.
The actual number of women who experience complications may be under-reported, so while some women experience the benefits from implants, other women experience any or all of these complications as they are listed below from Australia’s Therapeutic Goods Administration (TGA) website: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
-punctures or lacerations of vessels, nerves, structures or organs, including the bladder, urethra or bowel (these may require surgical repair
-transitory local irritation at the wound site
-a ‘foreign body response’ (wound breakdown, extrusion, erosion, exposure, fistula formation and/or inflammation)
-mesh extrusion, exposure, or erosion into the vagina or other structures or organs
-as with all foreign bodies, mesh may potentiate an existing infection
-over-correction (too much tension applied to the tape) may cause temporary or permanent lower urinary tract obstruction
-acute and/or chronic pain
-voiding dysfunction
-pain during intercourse
-neuromuscular problems including acute and/or chronic pain in the groin, thigh, leg, pelvic and/or abdominal area
-recurrence of incontinence
-bleeding including haemorrhage, or haematoma
-seroma
-urge incontinence
-urinary frequency
-urinary retention
-adhesion formation
-atypical vaginal discharge
-exposed mesh may cause pain or discomfort to the patient’s partner during intercourse
-mesh migration
-allergic reaction
-abscess
-swelling around the wound site
-recurrent prolapse
-contracture
-scarring
-excessive contraction or shrinkage of the tissue surrounding the mesh
-vaginal scarring, tightening and/or shortening
-constipation/defecation dysfunction
-granulation tissue formation.
I've been told that it is a new type of mesh, or that it's a sling. Is this the same?Mesh, tape, sling - it is all polypropylene mesh. It is a complex area and rapidly changing so clinicians may not be aware that they are in essence, all the same. If you don't want mesh, you have the right to request native tissue repair or a procedure like a Burch colposuspension. It is your body and you need to feel confident you are providing informed consent.
What are the alternatives to using mesh for incontinence and prolapse?Non-surgical options includes physiotherapy and pessaries. Surgery should be considered a last resort when all other options have been exhausted.
There are surgical options which don't include mesh such as Native Tissue Repair and Burch Colposuspension. Have a look at the Australian Commission on Safety and Quality in Healthcare's resources on this page for Pelvic Organ Prolapse and Stress Urinary Incontinence and remember the key advice that surgery should be the last resort when all other options have been exhausted.
You will be the one who will bear the consequences if you do have complications from the mesh, so it's important that you provide informed consent. The Choosing Wisely campaign has created these questions to help you get started. http://www.choosingwisely.org.au/resources/consumers/5-questions-to-ask-your-doctor - plus it is useful to ask how many of the same procedures your surgeon has done, and what the outcomes have been. Any reluctance to answer this question may signal you have not found the right surgeon for you.
Is mesh banned?No it is not banned. It has been banned for some, but not all types of pelvic organ prolapse surgery, but for the most common surgery, stress urinary incontinence, it has not been banned. From 1 December 2018, all new surgical mesh devices seeking approval from the TGA will need to meet the higher evidentiary requirements of a Class III medical device. This does not apply to mesh devices already on the TGA register however.
Can I get the mesh taken out?It is very difficult to fully remove mesh. Women are offered partial removals of mesh, for example snipping of the part protruding through the vaginal wall. Many women do not want partial removals as the remaining mesh frays and causes ongoing issues, and it may be more difficult to get the rest of the mesh out. Some women have taken the decision to self-fund and travel overseas to where other surgeons more experienced in full mesh removal may be able to provide assistance. We are continuing to work on this as a nation and the options are continually evolving. The WA Pelvic Mesh Support Group can be an important source of support to find out latest options, or you can call the Health Consumers Council on 9221 3422/ 1800 620 780 for country callers, or email info@hconc.org.au
What help is available for women?- You can call the WA Pelvic Mesh Clinic line at King Edward Hospital on 1800 962 202. This is answered from 8.30-4pm Monday to Friday, with a Message Bank for after hours or when the line is busy. The person answering the phone is not a doctor, nurse or midwife. You will be linked with the Mesh Clinic for an appointment if appropriate. Unfortunately there are currently long waiting times for appointments.
- In WA there is the WA Pelvic Mesh Support Group which can connect you with women who have had these procedures
- Take this information sheet to your trusted health provider to discuss your current or future options
What has been done about regulating mesh?The Therapeutic Goods Administration (TGA) regulates medications and medical devices. However, the evidence required to register a device is by no means as comprehensive as that required to register a medication.
What can I do to report complications?You can register your complications on The Therapeutic Goods Administration (TGA) website here: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
You can also call the Mesh Line if you are in WA on 1800 962 202
What happened about the Senate Inquiry into mesh?A Senate Inquiry into pelvic mesh was held in 2017, and the Recommendations have largely been accepted by our nation's Health Minister, who apologised to women harmed by mesh implants. They are currently in the early stages of being implemented, and health consumer councils across Australia are working with key bodies to ensure that there is a more consistent approach across Australia.
What about hernia mesh?Hernia mesh is emerging as the next key area of interest. The complications are very similar, as is the negative impact on people, and the difficulties they can face in getting help. A new peer group has been started in WA - Mesh Too Western Australia.
Pelvic Mesh refers to polypropylene mesh implants to treat women treated for stress urinary incontinence or pelvic organ prolapse.
Complications include pain, inflammatary reactions to the mesh, persistent infections, bleeding, with the mesh kinking, moving or migrating and causing damage to surrounding organs.
The actual number of women who experience complications may be under-reported, so while some women experience the benefits from implants, other women experience any or all of these complications as they are listed below from Australia’s Therapeutic Goods Administration (TGA) website: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
-punctures or lacerations of vessels, nerves, structures or organs, including the bladder, urethra or bowel (these may require surgical repair
-transitory local irritation at the wound site
-a ‘foreign body response’ (wound breakdown, extrusion, erosion, exposure, fistula formation and/or inflammation)
-mesh extrusion, exposure, or erosion into the vagina or other structures or organs
-as with all foreign bodies, mesh may potentiate an existing infection
-over-correction (too much tension applied to the tape) may cause temporary or permanent lower urinary tract obstruction
-acute and/or chronic pain
-voiding dysfunction
-pain during intercourse
-neuromuscular problems including acute and/or chronic pain in the groin, thigh, leg, pelvic and/or abdominal area
-recurrence of incontinence
-bleeding including haemorrhage, or haematoma
-seroma
-urge incontinence
-urinary frequency
-urinary retention
-adhesion formation
-atypical vaginal discharge
-exposed mesh may cause pain or discomfort to the patient’s partner during intercourse
-mesh migration
-allergic reaction
-abscess
-swelling around the wound site
-recurrent prolapse
-contracture
-scarring
-excessive contraction or shrinkage of the tissue surrounding the mesh
-vaginal scarring, tightening and/or shortening
-constipation/defecation dysfunction
-granulation tissue formation.
Mesh, tape, sling - it is all polypropylene mesh. It is a complex area and rapidly changing so clinicians may not be aware that they are in essence, all the same. If you don't want mesh, you have the right to request native tissue repair or a procedure like a Burch colposuspension. It is your body and you need to feel confident you are providing informed consent.
Non-surgical options includes physiotherapy and pessaries. Surgery should be considered a last resort when all other options have been exhausted.
There are surgical options which don't include mesh such as Native Tissue Repair and Burch Colposuspension. Have a look at the Australian Commission on Safety and Quality in Healthcare's resources on this page for Pelvic Organ Prolapse and Stress Urinary Incontinence and remember the key advice that surgery should be the last resort when all other options have been exhausted.
You will be the one who will bear the consequences if you do have complications from the mesh, so it's important that you provide informed consent. The Choosing Wisely campaign has created these questions to help you get started. http://www.choosingwisely.org.au/resources/consumers/5-questions-to-ask-your-doctor - plus it is useful to ask how many of the same procedures your surgeon has done, and what the outcomes have been. Any reluctance to answer this question may signal you have not found the right surgeon for you.
No it is not banned. It has been banned for some, but not all types of pelvic organ prolapse surgery, but for the most common surgery, stress urinary incontinence, it has not been banned. From 1 December 2018, all new surgical mesh devices seeking approval from the TGA will need to meet the higher evidentiary requirements of a Class III medical device. This does not apply to mesh devices already on the TGA register however.
It is very difficult to fully remove mesh. Women are offered partial removals of mesh, for example snipping of the part protruding through the vaginal wall. Many women do not want partial removals as the remaining mesh frays and causes ongoing issues, and it may be more difficult to get the rest of the mesh out. Some women have taken the decision to self-fund and travel overseas to where other surgeons more experienced in full mesh removal may be able to provide assistance. We are continuing to work on this as a nation and the options are continually evolving. The WA Pelvic Mesh Support Group can be an important source of support to find out latest options, or you can call the Health Consumers Council on 9221 3422/ 1800 620 780 for country callers, or email info@hconc.org.au
- You can call the WA Pelvic Mesh Clinic line at King Edward Hospital on 1800 962 202. This is answered from 8.30-4pm Monday to Friday, with a Message Bank for after hours or when the line is busy. The person answering the phone is not a doctor, nurse or midwife. You will be linked with the Mesh Clinic for an appointment if appropriate. Unfortunately there are currently long waiting times for appointments.
- In WA there is the WA Pelvic Mesh Support Group which can connect you with women who have had these procedures
- Take this information sheet to your trusted health provider to discuss your current or future options
The Therapeutic Goods Administration (TGA) regulates medications and medical devices. However, the evidence required to register a device is by no means as comprehensive as that required to register a medication.
You can register your complications on The Therapeutic Goods Administration (TGA) website here: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
You can also call the Mesh Line if you are in WA on 1800 962 202
A Senate Inquiry into pelvic mesh was held in 2017, and the Recommendations have largely been accepted by our nation's Health Minister, who apologised to women harmed by mesh implants. They are currently in the early stages of being implemented, and health consumer councils across Australia are working with key bodies to ensure that there is a more consistent approach across Australia.
Hernia mesh is emerging as the next key area of interest. The complications are very similar, as is the negative impact on people, and the difficulties they can face in getting help. A new peer group has been started in WA - Mesh Too Western Australia.
My Baby WA Pregnancy App
The My Baby WA app launched in June 2021 withy a massive initial response.
The app was developed through a partnership between the WA Country Health Service and Health Consumers’ Council Wa. The app is to assist women and families to navigate the pregnancy, birth and early parenting periods- providing information that is specific for women and families in Western Australia.
My Baby WA provides pregnant women and families in Western Australia accessible and evidence based information during their pregnancy. Functions on the app include;
· All the information you need on pregnancy, birth and your baby
· A WA maternity service locator including models of care available at each service
· Week by week pregnancy information
· An interactive timeline for women to track their appointments, tests, screening and education offered to them during their pregnancy
· A baby bump photo gallery
· Noongar lullabies to play and sing to your unborn baby
· Option to fill in the Women’s Experiences of Maternity Services to Survey to provide feedback to you maternity service.
· Mum and Partner modes for pregnancy, birth and early parenting tips
The app can be downloaded on iPhone or Android.
International Patient Safety Day Q&A Panel – Maternal and newborn safety
To mark World Patient Safety Day 2021, and the theme of safe maternal and newborn care, in partnership with AHPRA and Women’s and Newborns Health Network, Health Consumers’ Council convened a Q&A panel discussion exploring maternal and childbirth care.
We explored topics such as Aboriginal women’s experiences of childbirth, the impact of COVID on birthing women, why women and families’ feedback is important and how it changes things. We also confirmed the importance of education, and of involving birthing women and families at all stages and at all levels in designing and evaluating maternity services.
Listen on catch-up (1.5 hours)
National Strategic Approach to Maternity Services
We have been involved with this national strategy as much as possible, although it has been some time since there was an update. You can find out more about maternity services in Australia here.