World Tuberculosis Day
Today is World Tuberculosis (TB) Day, 2017 is the second year of the “Unite to End TB” campaign. The UN Sustainable Development Goals and the WHO End TB Strategy target is to end TB by 2030. Click here to read more about World Tuberculosis Day and how you can support the “Unite to End TB” and “Leave No One Behind” campaigns.
The following article, first published in Health Matters Magazine in 2016, written by Majok Wutchok, (a member of the Sudanese community in Perth) outlines how West Australian Tuberculosis Control Program could be improved from a consumer perspective.
Tuberculosis (TB) is considered the second most deadly disease after HIV/AIDS in developing countries. Every year there is a mass movement of Australian’s travelling overseas on holiday and returning home. A major concern is there isn’t proper health promotion and public health education to protect consumers when they and their relatives return from overseas. Due to the lack of public health education they and their family may not be aware they are coming home infected with a tropical or communicable disease.
I recommend the WA Health Department set up a consumer overseas travellers screening task force, to avoid a future catastrophic spread of disease across the state. There is also a need to engage with healthcare providers to empower those infected with Tuberculosis and other communicable diseases and to support and empower their community.
Western Australia Tuberculosis Control Program
The current program, ‘Western Australia Tuberculosis Control Program’ is administered by the North Metropolitan Area Health Service (NMAHS). However, the program only endeavours to screen and treat the disease once it has been acquired, it does nothing to educate those at risk on prevention methods. ‘Western Australia Tuberculosis Control Program’ detailed as follows:
‘The program manages Tuberculosis in Western Australia and offers a state-wide public health service that operates as a resource centre and clinic. Aspects of the service include:
- Treatment of Active TB: Diagnosis, treatment and case management
- Surveillance and prevention of TB
- Active screening of high risk groups
- Contact tracing
- Diagnosis and treatment of latent TB infection (preventative therapy)
- Tuberculin Skin Test (TST), also known as Mantoux testing and BCG vaccinations to selected populations. Training and accreditation can be provided for relevant health professionals.
- Free Health Service: All services related to the diagnosis, treatment of TB and relevant medications are provided at no charge. (See “Fees and charges related to the diagnosis and management of tuberculosis and leprosy” (Operational Directive OD 0229/09))
- TB Infection Control
- Advice on pre-employment screening of Health Care Workers and Tertiary Students
- Advice on Management of TB risk in health care settings
- Assistance with contact tracing in health care settings
- Hansen’s Disease (Leprosy): Outpatient clinic service and consultative advice
- Consultation: Specialist advice from medical and nursing staff is readily available, including preventative advice, health service education and access to information programs.
- Policy and Operational Directives: Develop, implement and review policy relevant to TB management and control
- TB Notification and Enhanced Surveillance data base: Maintenance and reporting on TB epidemiology’
(http://www.health.wa.gov.au/acc/tb/)
Prevention is better than Cure
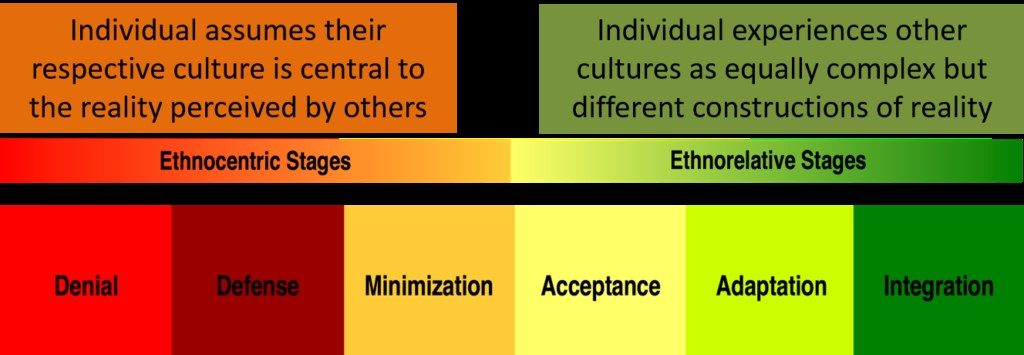
Even in 1918 the thinking regarding Tuberculosis, was ‘Prevention is better than a cure’ (Cobbett, L 1918, British Journal of Tuberculosis, vol. 12, no. 1, pp. 16-19). According to the World Health Organisation (WHO 2014), prevention strategies involve encouraging and conducting research. It has been suggested that integrated intervention programs with consumers and their communities involved can be very beneficial. As opposed to vertical programs which are considered limited, integrated programs are considered far more effective for prevention. However, integrated programs need established communication and consistent health education together with consumers’ participation across all aspects.
Engaging Consumers is the key
Regarding primary healthcare and consumers, the involvement of a population group from high-risk consumers is paramount. At the same time public health education and community health promotion are also considered important, and are associated with the continuous use of those preventive measures by the consumer’s communities.
In short it is important sustainable prevention measures are taken to educate those at risk, to prevent them catching Tuberculosis and other communicable diseases while travelling, rather than simply screening and treating the disease when it has already been contracted.
Majok Wutchok | Consumer Representative | ANUTR | MPH Student
(This article was first published as ‘Consumer Approach Vs Tuberculosis Control in WA’ in HCC Health Matters Magazine 2016 Issue 2)
If you would like assistance partnering with consumers in health, the HCC Consumer & Community Engagement Team can help!
Partnering With Consumers
HCC facilitates on-site workshops that assist health care staff to increase their understanding of effective partnering with consumers in the governance and operational structures of your organisation. Principles of consumer participation within the context of health service accreditation can also be a key component of this bespoke fee for service training. Training can be conducted specifically for board members, executive committee members, management and point of care delivery staff, or with a whole of organisation approach.
Safety And Quality Committees
We can provide new and existing consumer members with information on the elements of quality and why patient safety is a critical area of focus in health care. This fee for service training can be tailored to meet the needs of specific safety and quality committees.
Register Your Interest
Please complete the form here to register your interest in HCC’s workshops.
For Further Information
Please contact the Health Consumers Council Community and Consumer Engagement team on 9221 3422 or email:
Louise Ford: louise.ford@hconc.org.au
Steph Newell: stephanie.newell@hconc.org.au