By Pip Brennan, Health Consumers’ Council Executive Director
On Saturday 20th July I attended an event in the community, run by the Uniting Church on the Voluntary Assisted Dying Bill. One of the speakers was Emma-Jade Sanderson, who is the Chair of the Joint Select Committee on End of Life Choices. The My Life My Choices Report from this committee is a weighty 600 pages, and a 16-page summary of the report and the response from the current government is also available.
As we noted in pages 9-10 of our Autumn edition of Health Matters, there are divergent views on end of life choices. A key concern from disability advocate Sam Connor was the systemic discrimination of people with disabilities, and the plea to be assisted to live, before being assisted to die.
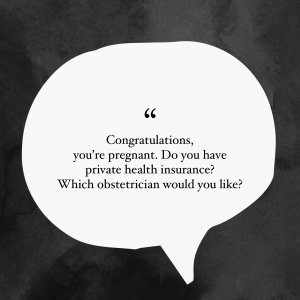
Our submission to the WA Voluntary Assisted Dying Legislation Consultation echoed this concern. We also noted that “In truth, VAD is going to be accessible to very few people.” What is going to make the most difference to the most West Australians we believe, is access to good quality palliative care.
It would be wonderful if palliative care had more positive community connotations – about living well, having choice and comfort from distressing symptoms.
So I took great heart from Amber-Jade Sanderson’s reflection that whenever there is a focus on voluntary assisted dying in any jurisdiction around the world, more focus and funding is put onto palliative care. And right now there are important opportunities to influence palliative care/ quality of life care.
Your opportunity to have a say on Palliative Care
Summit
On Saturday 24th August there is an important opportunity to have your say on palliative care. A summit is being convened at the Perth Convention and Exhibition Centre:
- 7am Breakfast
- 9am Summit
You can book for both (“with breakfast” option), or just for the Summit (“without breakfast”) option.
This is an opportunity to bring together everyone interested in the delivery of palliative care in Western Australia – Health professionals, general practitioners, palliative care specialists, health consumers and carers. It aims to shape how we put into practice Recommendations 7-18 of the My Life My Choices Report, the Palliative Care Strategy 2018 – 2028 and relevant Sustainable Health Review Report 2018 Recommendations. Attendees are encouraged to share their experiences to provide insight and influence the provision of high quality palliative care for all Western Australians. It is a partnership event with Palliative Care WA, WA Country Health Service, WA Primary Health Alliance, Palliative and Supportive Care Education and the Health Consumers’ Council of WA.
An additional session will be held by video conference from multiple sites across regional WA for those unable to travel to Perth on Monday 19 August from 10am to 1.00pm.
Please note that the registration form requires you to complete the job title and place of work. You can just complete “Consumer” or “Carer” for both Job Title and Company/ Organisation. For address you can complete your own address or write the words “Home Address” if you don’t want to complete this information. You can repeat your home number or mobile number for Work Phone.
Register HereSurvey
Whether or not you want to attend, you can have your say in this short survey – you can have a look at the questions here before you jump online and complete the survey.
Complete the survey here