 The planned new subsidy scheme for Perth Children’s Hospital is the subject of this ABC news article which reveals that there will no longer be free parking for any families, and that the new rebate scheme, which may support more families, will cost $5 per day. Those who are not eligible for the rebate will pay $21.30 per day
The planned new subsidy scheme for Perth Children’s Hospital is the subject of this ABC news article which reveals that there will no longer be free parking for any families, and that the new rebate scheme, which may support more families, will cost $5 per day. Those who are not eligible for the rebate will pay $21.30 per day
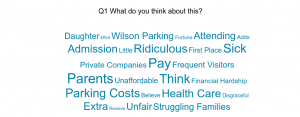
We asked you to complete a survey about parking, and more than a 100 of you responded. The first question we asked is “What do you think?” and received an overwhelming response that this was not OK. The full ten pages of comments are here. This is what you said, in a nuts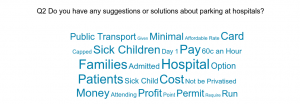 hell:
hell:
- Parents of sick children are already under stress. They shouldn’t have to worry about parking too
- Parking shouldn’t have been privatised in the first place
- There should be a CAT bus which goes past the Perth Children’s Hospital
We also asked you what you thought could be done, and received seven pages of comments you can read here.
And we were reminded that NSW drastically cut the cost of hospital parking after a petition was started by a young patient, and so did Queensland and it was only just over a year ago that WA’s Nathan Garcia protested his mother Monique Garcia’s parking fine of $1,000 which prompted a national petition, now closed, for free hospital parking. It is a big nut to crack, hospital parking, as there are complications such as free parking being mis-used by people not attending the hospital (which obviously can be overcome by ticketing technology), and considerations of how the cost of maintaining the car park will be met (e.g. in loss of clinical services) and so on. But it is a conversation we need to keep having.
Next steps
- We will contact those of you who said you would like to keep in touch with us about this issue.
- The CAT bus is an idea worth pursuing and HCC will follow this up.
- Other options such as corporate partnerships to cover the cost also need to be explored. We will keep you posted…