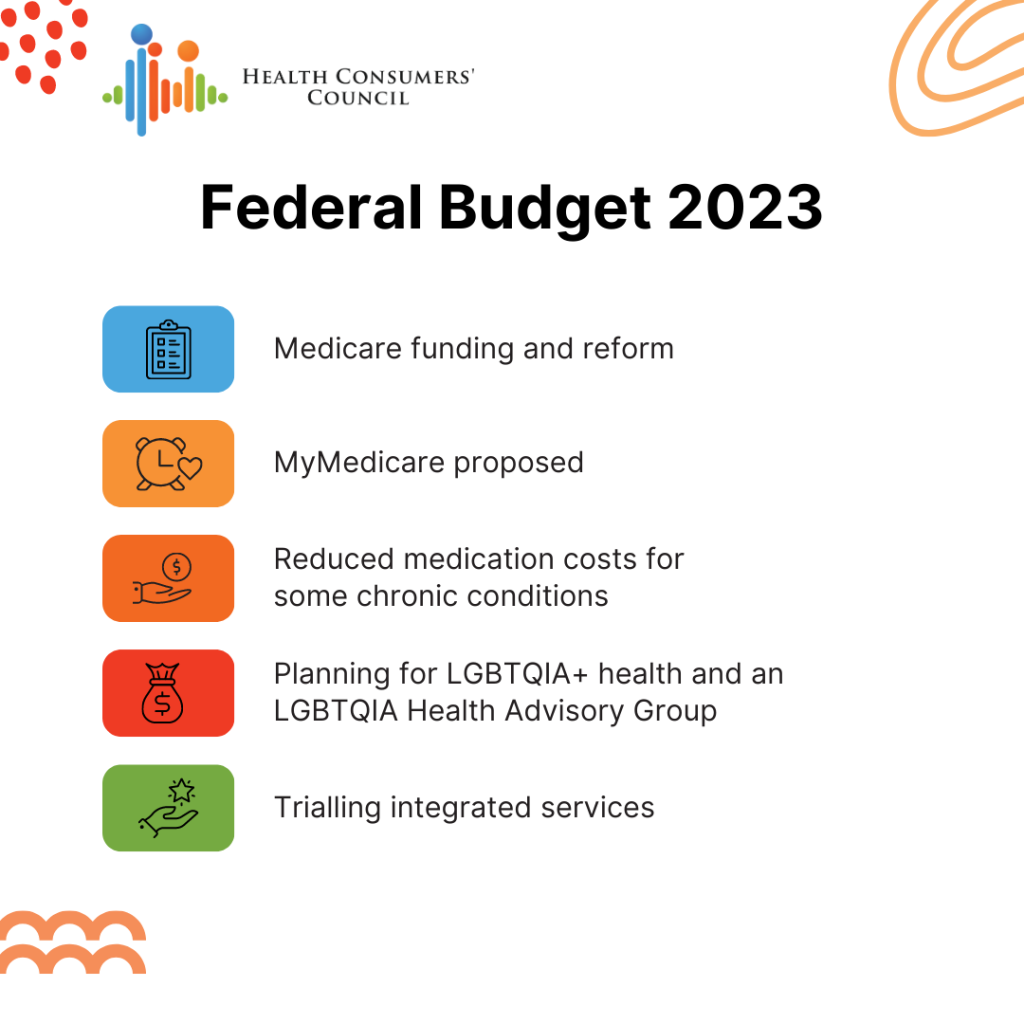
Health Consumers’ Council is encouraged by the reforms announced in the Federal Budget 2023-24 that will give consumers better access to affordable primary care (GP) services. Some of the highlights of the budget include:
- Medicare funding and reform to improve access to primary care:
- Increased incentives for GPs to offer bulk-billing for patients under 16 years old and concession card holders
- Funding to better engage health consumers in primary care reform, mental health services, and multicultural healthcare
- Improved investment in preventative healthcare for Aboriginal people
- New urgent care clinics to take the pressure off emergency departments
- Savings on around 300 medications, with consumers able to buy two months’ supply at a time
- MyMedicare – a new voluntary scheme to create a stronger relationship between patients and their primary care teams allowing for better continuity of care and easier access to telehealth consultations
- Trialling integrated service and joint commissioning across the primary health system, disability care, aged care, First Nations health, and veterans’ care
- Funding allocated to commence planning for LGBTQIA+ health and form an LGBTQIA Health Advisory Group
However, HCC believes more detail is needed about the implementation and application of the proposed MyMedicare, as there may be an equity issue for consumers who could benefit from the associated services, such as longer telehealth sessions, but may experience digital exclusion. There is a concern that this may create a two-tier system within Medicare, which would disadvantage some consumers.
There were also some notable funding gaps related to allied services and dental health, a disappointing lack of focus on climate change and its health impacts, a lack of services related to COVID outside of vaccines and diagnosis, and insufficient focus on preventative health measures.
What we do know is that there’s going to be some big changes in the coming months and years with all of the reforms happening in health and social care, and we look forward to ensuring the consumer voice is at the centre of health policy and service delivery.
If you want to know more about the Budget 2023-24, or you have questions for the Federal Minister for Health and Aged Care, you can join Consumers Health Forum of Australia for an interactive online webinar, Q&A style, on Friday 9 June, 8:30-9:30am WST.
Find out more, and register, here.
National Health Reform Agreement
In other health reform news, the Federal Government has commissioned an independent review of The National Health Reform Agreement, an agreement between between the Commonwealth government and the state government on a range of health issues.
Health Consumers’ Council will be submitting a response to the review, you can read more about it here.