
Search Results for: mesh
Senate Inquiry into Pelvic Mesh – A Scandal of International Proportions
 On Wednesday 28th March, one day late, the Senate Inquiry into the “Number of women in Australia who have had transvaginal mesh implants and related matters” handed down is final report. The Senate Inquiry was championed by Derryn Hinch, who called pelvic mesh “the biggest medical scandal for Australian women since thalidomide in the 1950s and 1960s, when kids were born without arms and legs”.
On Wednesday 28th March, one day late, the Senate Inquiry into the “Number of women in Australia who have had transvaginal mesh implants and related matters” handed down is final report. The Senate Inquiry was championed by Derryn Hinch, who called pelvic mesh “the biggest medical scandal for Australian women since thalidomide in the 1950s and 1960s, when kids were born without arms and legs”.
Derryn Hinch had listened to the voices of the Australian Pelvic Mesh Support Group women who campaigned tirelessly to be heard. He was able to get the Senate Inquiry convened, and the hope was that the Senate Inquiry would raise awareness of the permanent, life-altering consequences for some women and call for a ban on its use. However, instead of a ban on the use of mesh, the Inquiry has recommended that mesh only be used “as a last resort”. This Media Release from the Australian Pelvic Mesh Support Group outlines the view of the women across Australia who have suffered permanent, life-altering consequences of pelvic mesh to the Inquiry Report:
There are a few glimmers of hope for mesh-injured women in the report – but the wording used in the recommendations are so weak that it could, if not followed up by robust policy change, give Australian health authorities, specialists and primary carers permission to carry on as usual.
This article summarises the Inquiry Report and highlights the critical importance of always asking the questions you need to provide informed consent. It is simplistic to say that your doctor only has your best interests at heart. There are many other factors at play, as this pelvic mesh scandal has shown.
Complications
Chapter Two of the Inquiry’s Report is a must-read. It documents women’s experiences of complications from mesh implants, compounded by an inability or unwillingness of the medical profession to hear and respond to these reports. At great personal cost, women attended the Senate Inquiry hearings to tell their story:
I presented with mild stress incontinence with exercising and 2 years on I have total and uncontrollable urinary incontinence. I have had multiple hospital admissions, surgeries, invasive investigations and a total loss of my pride as a woman. Name withheld, Submission 458, p. [6].
I dragged myself to work each day and on weekends I was bedridden. I was unable to do normal things like shopping, cooking and housework without debilitating pain and fatigue. My relationship with my family, friends suffered as I could not handle social activities. Not being able to care for my new grandson broke my heart. Surfing was impossible and walking the dogs or doing other light physical exercise was just too painful. Name withheld, Submission 67, p. 1.
To this day, women will still be told “it’s not the mesh” by their GPs and specialists. Even by clinicians working in Mesh Clinics.
Consent
Does it seem peculiar that a Senate Inquiry would spell out the process for ensuring that patients provide informed consent to having a procedure? And yet that is exactly what Recommendation 6 addresses:
The committee recommends that the Australian Commission on Safety and Quality in Health Care prepare guidance material on effective informed consent processes, with a view to ensuring that a dialogue between a medical practitioner and patient should:
- clarify the rationale for the proposed treatment;
- discuss the range of alternate treatment options available and their attendant risks and benefits;
- discuss the likely success and potential complications of the recommended treatment as they relate to the individual patient;
- provide an opportunity for the patient to ask questions; and
- confirm that the individual patient has understood the information discussed.
Here is one consent conversation, which was echoed in many of the submissions and evidence given to the Senate Inquiry:
I was told by my implanting surgeon that I would be back at the gym within 10 days post implant procedure and that I would be like a 16-year-old virgin after the implants. Committee Hansard, 18 September 2017, p. 1.
And many other women simply do not know they have been implanted with mesh. Here is another, common reflection from a woman in a submission to the Inquiry:
How can I have not known a foreign medical device had been implanted in my body without my consent? Name withheld, Submission 528, p. [1]
Reporting complications
There are key barriers to the reporting of complications:
1) it is not mandatory for clinicians to report complications:
…based on my experience and that of many other women in this town, I would not trust surgeons to report complications or gather accurate research data. We all have similar stories of complications, including crippling pain and terrible bowel and bladder symptoms, which were trivialised or denied, and we were told we were the only one with an adverse outcome, that it was our fault that our body had reacted to the mesh. We were abandoned by our surgeon and left to cope as best we could. Kathryn, Committee Hansard, 19 September 2017, p. 4.
2) women are simply not believed when they report complications:
The problem is acknowledging the symptoms in the first place, though. There are a lot of GPs who won’t acknowledge it and there are a lot of gynaecologists who won’t acknowledge it… How can they report it if they’re not acknowledging that your pain and complications are from your mesh? Carolyn Chisholm, Committee Hansard, 25 August 2017, p. 9.
3) it is a complex non-consumer friendly process, requiring the serial number of the mesh implant, which most women won’t have without getting their medical records, which may no longer be available:
Although I am interested in reporting the adverse events I have experienced to the TGA, the TGA Users Medical Device Incident Report is daunting and I simply do not have the detailed information they request for device identification… I have encountered obstacles in trying to obtain my medical records. Name withheld, Submission 477, p. 3.
Medical Device Companies – driving uptake
Prior to my involvement in this issue, I had no idea that medical device companies are the bodies that train clinicians in how to use them. Effectively, they can drive demand for their own product:
The sponsoring companies actively promote medical specialists who utilise their products to referring GPs and company-sponsored educational activities, where one of the aims of that activity is to increase utilisation of those products. Sponsoring companies are also actively involved in the education and provision of training to
medical specialists. Associate Professor Christopher Maher, Committee Hansard, 19 September 2017, p. 30.
What about women who have been injured by mesh?
Every aspect of women’s lives are impacted when there are severe complications. Inability to work means significant economic disadvantage. Sexual dysfunction can mean the end of a relationship. Pain robs life of its quality. Accessing medical assistance is hugely problematic when there is a lack of acceptance that the symptoms are related to mesh, and the lack of actual services. Mesh removal services are very patchy, and some women were advised that mesh removal would mean a colostomy for life. Women have voted with their feet and travelled to the US to access specialist mesh removal care which has not resulted in this awful choice between removal and a functioning bowel. The surgery is significant and the outcomes are uncertain. There is no guarantee the debilitating pain will cease once the mesh is removed.
The final Recommendation tries to address the range of impacts on women:
Recommendation 13: The committee recommends that State and Territory governments continue to work with the Australian Commission on Safety and Quality in Health Care to review the provision of services for the use and removal of transvaginal mesh devices. In particular, the committee recommends that consideration be given to the establishment of:
- information and helplines that women who have received transvaginal mesh implants can contact for advice on the availability of treatment and support services, including financial support programs, in their state;
- specialist counselling programs, to assist women who have sustained injuries following transvaginal mesh procedures;
- specialist multidisciplinary units for the assessment and management of complications associated with transvaginal mesh procedures, comprising:
- comprehensive diagnostic procedures, including relevant diagnostic imaging facilities and expertise;
- specialist pain management expertise; and
- high level expertise in the partial or full removal of transvaginal mesh;
- advice and practical assistance for women who are seeking to access their medical records
The Health Consumers’ Council of WA is aware that many women impacted by mesh implants are seeking full removals, not partial removals. The reality is at present that there are few surgeons, if any, who can perform full removals in Australia. Women have completely lost trust in the clinicians who implanted them in the first place now assuring them that the mesh will be fully removed. Since the Inquiry has finished, we are aware of women who have sought imaging after enduring full removal procedures only to discover there is still mesh inside them.
Western Australia
Women in Western Australia are referred to this page on the Health Consumers Council website for up to date information. This is an area which is rapidly changing. Please contact HCC on 9221 3422 during office hours if further support is required.
Written by Pip Brennan, Executive Director of the Health Consumers’ Council (WA) Inc.
Mesh Implants
A GLOBAL HEALTH CRISIS – PELVIC MESH IMPLANTS
It has taken some time for the scale and extent of the impact of pelvic mesh implants for women to treat stress urinary incontinence and pelvic organ prolapse. Once hailed as the perfect solution for an enduring surgical fix for these non-life-threatening conditions, it has left a swathe of women with permanent, life altering consequences. Persistent pelvic pain at rest. Inability to have sex. Inability to continue working, and the financial impact often amplified by failed marriages as the lack of intimacy took its toll. The full list of complications is listed on the Therapeutic Goods Administration mesh hub.
In 2017 Australia undertook a Senate Inquiry – entitled Number of women in Australia who have had transvaginal mesh implants and related matters. We literally did not know how many women had been impacted. There were 13 recommendations in the final report, with a mix of federal and state responsibilities to effect implementation. There was even one on effective informed consent processes. It was clear from submissions and hearings that women were not informed about the potential horrific consequences of their choice, and that the mesh is extremely complex to remove. With the divide of responsibility between state and federal governments and the fact that most of the implant surgeries were performed in private hospitals, it is difficult to track real progress. Some meshes have been banned from use, but by no means all. Many women are still unaware that their sequelae of symptoms are related to their mesh implants. GPs and specialists may also be unaware.
WA PELVIC MESH SUPPORT GROUP
The peer support group the WA Pelvic Mesh Support Group has its own website and is an essential stakeholder in WA’s response to the mesh crisis.
WA PELVIC MESH COMPLICATIONS CLINIC
This clinic has been set up in King Edward Memorial Hospital and has been operating since 2017. There is a committee of clinicians and consumers who meet to discuss the clinic’s model and progress, as this area is complex and changing. The committee continues to aim to advance the recommendations of the Inquiry.
UNFINISHED BUSINESS – A NATIONAL FORUM ON THE IMPACT OF MESH IMPLANTS
 A National Mesh Implant Forum was held in Melbourne on Friday April 5, 2019, to consider all aspects of Australia’s mesh implant crisis. The Forum was proudly convened by the Health Issues Centre and Health Consumers NSW, Health Consumers Queensland, Health Consumers’ Council (WA), Health Consumers Alliance of South Australia, Health Care Consumers (ACT), Health Consumers Tasmania.
A National Mesh Implant Forum was held in Melbourne on Friday April 5, 2019, to consider all aspects of Australia’s mesh implant crisis. The Forum was proudly convened by the Health Issues Centre and Health Consumers NSW, Health Consumers Queensland, Health Consumers’ Council (WA), Health Consumers Alliance of South Australia, Health Care Consumers (ACT), Health Consumers Tasmania.
The event brought together mesh injured consumers, carers, regulatory authorities, health officials, the Chair of the Senate Inquiry into mesh and consumer advocates to create solutions and bring about real change. The forum considered not only the impact of pelvic mesh, but the emerging parallel crisis involving people who have received hernia mesh implants. A full report is available here.
NEW REPORT – HERNIA MESH IMPLANTS – CONSUMER SURVEY
Health Issues Centre Victoria initiated the Mesh Device and Implant Failure study late last year and of the respondents, a sizeable 183 patients have already reported major problems with their hernia mesh implants. 70 per cent of these are men. You can read the report here.
According to publicly available figures nearly 100,000 Australians are hospitalised for hernia each year. However, the numbers of patients that go on to have pelvic mesh implants and that are negatively impacted is not known. People who would like to report complications of hernia procedures using mesh can complete the survey here.
PELVIC MESH FAQs
What is pelvic mesh?Pelvic Mesh refers to polypropylene mesh implants to treat women treated for stress urinary incontinence or pelvic organ prolapse.
What are the complications of pelvic mesh?Complications include pain, inflammatary reactions to the mesh, persistent infections, bleeding, with the mesh kinking, moving or migrating and causing damage to surrounding organs.
The actual number of women who experience complications may be under-reported, so while some women experience the benefits from implants, other women experience any or all of these complications as they are listed below from Australia’s Therapeutic Goods Administration (TGA) website: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
-punctures or lacerations of vessels, nerves, structures or organs, including the bladder, urethra or bowel (these may require surgical repair
-transitory local irritation at the wound site
-a ‘foreign body response’ (wound breakdown, extrusion, erosion, exposure, fistula formation and/or inflammation)
-mesh extrusion, exposure, or erosion into the vagina or other structures or organs
-as with all foreign bodies, mesh may potentiate an existing infection
-over-correction (too much tension applied to the tape) may cause temporary or permanent lower urinary tract obstruction
-acute and/or chronic pain
-voiding dysfunction
-pain during intercourse
-neuromuscular problems including acute and/or chronic pain in the groin, thigh, leg, pelvic and/or abdominal area
-recurrence of incontinence
-bleeding including haemorrhage, or haematoma
-seroma
-urge incontinence
-urinary frequency
-urinary retention
-adhesion formation
-atypical vaginal discharge
-exposed mesh may cause pain or discomfort to the patient’s partner during intercourse
-mesh migration
-allergic reaction
-abscess
-swelling around the wound site
-recurrent prolapse
-contracture
-scarring
-excessive contraction or shrinkage of the tissue surrounding the mesh
-vaginal scarring, tightening and/or shortening
-constipation/defecation dysfunction
-granulation tissue formation.
I've been told that it is a new type of mesh, or that it's a sling. Is this the same?Mesh, tape, sling - it is all polypropylene mesh. It is a complex area and rapidly changing so clinicians may not be aware that they are in essence, all the same. If you don't want mesh, you have the right to request native tissue repair or a procedure like a Burch colposuspension. It is your body and you need to feel confident you are providing informed consent.
What are the alternatives to using mesh for incontinence and prolapse?Non-surgical options includes physiotherapy and pessaries. Surgery should be considered a last resort when all other options have been exhausted.
There are surgical options which don't include mesh such as Native Tissue Repair and Burch Colposuspension. Have a look at the Australian Commission on Safety and Quality in Healthcare's resources on this page for Pelvic Organ Prolapse and Stress Urinary Incontinence and remember the key advice that surgery should be the last resort when all other options have been exhausted.
You will be the one who will bear the consequences if you do have complications from the mesh, so it's important that you provide informed consent. The Choosing Wisely campaign has created these questions to help you get started. http://www.choosingwisely.org.au/resources/consumers/5-questions-to-ask-your-doctor - plus it is useful to ask how many of the same procedures your surgeon has done, and what the outcomes have been. Any reluctance to answer this question may signal you have not found the right surgeon for you.
Is mesh banned?No it is not banned. It has been banned for some, but not all types of pelvic organ prolapse surgery, but for the most common surgery, stress urinary incontinence, it has not been banned. From 1 December 2018, all new surgical mesh devices seeking approval from the TGA will need to meet the higher evidentiary requirements of a Class III medical device. This does not apply to mesh devices already on the TGA register however.
Can I get the mesh taken out?It is very difficult to fully remove mesh. Women are offered partial removals of mesh, for example snipping of the part protruding through the vaginal wall. Many women do not want partial removals as the remaining mesh frays and causes ongoing issues, and it may be more difficult to get the rest of the mesh out. Some women have taken the decision to self-fund and travel overseas to where other surgeons more experienced in full mesh removal may be able to provide assistance. We are continuing to work on this as a nation and the options are continually evolving. The WA Pelvic Mesh Support Group can be an important source of support to find out latest options, or you can call the Health Consumers Council on 9221 3422/ 1800 620 780 for country callers, or email info@hconc.org.au
What help is available for women?- You can call the WA Pelvic Mesh Clinic line at King Edward Hospital on 1800 962 202. This is answered from 8.30-4pm Monday to Friday, with a Message Bank for after hours or when the line is busy. The person answering the phone is not a doctor, nurse or midwife. You will be linked with the Mesh Clinic for an appointment if appropriate. Unfortunately there are currently long waiting times for appointments.
- In WA there is the WA Pelvic Mesh Support Group which can connect you with women who have had these procedures
- Take this information sheet to your trusted health provider to discuss your current or future options
What has been done about regulating mesh?The Therapeutic Goods Administration (TGA) regulates medications and medical devices. However, the evidence required to register a device is by no means as comprehensive as that required to register a medication.
What can I do to report complications?You can register your complications on The Therapeutic Goods Administration (TGA) website here: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
You can also call the Mesh Line if you are in WA on 1800 962 202
What happened about the Senate Inquiry into mesh?A Senate Inquiry into pelvic mesh was held in 2017, and the Recommendations have largely been accepted by our nation's Health Minister, who apologised to women harmed by mesh implants. They are currently in the early stages of being implemented, and health consumer councils across Australia are working with key bodies to ensure that there is a more consistent approach across Australia.
What about hernia mesh?Hernia mesh is emerging as the next key area of interest. The complications are very similar, as is the negative impact on people, and the difficulties they can face in getting help. A new peer group has been started in WA - Mesh Too Western Australia.
What is pelvic mesh?
Pelvic Mesh refers to polypropylene mesh implants to treat women treated for stress urinary incontinence or pelvic organ prolapse.
What are the complications of pelvic mesh?
Complications include pain, inflammatary reactions to the mesh, persistent infections, bleeding, with the mesh kinking, moving or migrating and causing damage to surrounding organs.
The actual number of women who experience complications may be under-reported, so while some women experience the benefits from implants, other women experience any or all of these complications as they are listed below from Australia’s Therapeutic Goods Administration (TGA) website: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
-punctures or lacerations of vessels, nerves, structures or organs, including the bladder, urethra or bowel (these may require surgical repair
-transitory local irritation at the wound site
-a ‘foreign body response’ (wound breakdown, extrusion, erosion, exposure, fistula formation and/or inflammation)
-mesh extrusion, exposure, or erosion into the vagina or other structures or organs
-as with all foreign bodies, mesh may potentiate an existing infection
-over-correction (too much tension applied to the tape) may cause temporary or permanent lower urinary tract obstruction
-acute and/or chronic pain
-voiding dysfunction
-pain during intercourse
-neuromuscular problems including acute and/or chronic pain in the groin, thigh, leg, pelvic and/or abdominal area
-recurrence of incontinence
-bleeding including haemorrhage, or haematoma
-seroma
-urge incontinence
-urinary frequency
-urinary retention
-adhesion formation
-atypical vaginal discharge
-exposed mesh may cause pain or discomfort to the patient’s partner during intercourse
-mesh migration
-allergic reaction
-abscess
-swelling around the wound site
-recurrent prolapse
-contracture
-scarring
-excessive contraction or shrinkage of the tissue surrounding the mesh
-vaginal scarring, tightening and/or shortening
-constipation/defecation dysfunction
-granulation tissue formation.
I've been told that it is a new type of mesh, or that it's a sling. Is this the same?
Mesh, tape, sling - it is all polypropylene mesh. It is a complex area and rapidly changing so clinicians may not be aware that they are in essence, all the same. If you don't want mesh, you have the right to request native tissue repair or a procedure like a Burch colposuspension. It is your body and you need to feel confident you are providing informed consent.
What are the alternatives to using mesh for incontinence and prolapse?
Non-surgical options includes physiotherapy and pessaries. Surgery should be considered a last resort when all other options have been exhausted.
There are surgical options which don't include mesh such as Native Tissue Repair and Burch Colposuspension. Have a look at the Australian Commission on Safety and Quality in Healthcare's resources on this page for Pelvic Organ Prolapse and Stress Urinary Incontinence and remember the key advice that surgery should be the last resort when all other options have been exhausted.
You will be the one who will bear the consequences if you do have complications from the mesh, so it's important that you provide informed consent. The Choosing Wisely campaign has created these questions to help you get started. http://www.choosingwisely.org.au/resources/consumers/5-questions-to-ask-your-doctor - plus it is useful to ask how many of the same procedures your surgeon has done, and what the outcomes have been. Any reluctance to answer this question may signal you have not found the right surgeon for you.
Is mesh banned?
No it is not banned. It has been banned for some, but not all types of pelvic organ prolapse surgery, but for the most common surgery, stress urinary incontinence, it has not been banned. From 1 December 2018, all new surgical mesh devices seeking approval from the TGA will need to meet the higher evidentiary requirements of a Class III medical device. This does not apply to mesh devices already on the TGA register however.
Can I get the mesh taken out?
It is very difficult to fully remove mesh. Women are offered partial removals of mesh, for example snipping of the part protruding through the vaginal wall. Many women do not want partial removals as the remaining mesh frays and causes ongoing issues, and it may be more difficult to get the rest of the mesh out. Some women have taken the decision to self-fund and travel overseas to where other surgeons more experienced in full mesh removal may be able to provide assistance. We are continuing to work on this as a nation and the options are continually evolving. The WA Pelvic Mesh Support Group can be an important source of support to find out latest options, or you can call the Health Consumers Council on 9221 3422/ 1800 620 780 for country callers, or email info@hconc.org.au
What help is available for women?
- You can call the WA Pelvic Mesh Clinic line at King Edward Hospital on 1800 962 202. This is answered from 8.30-4pm Monday to Friday, with a Message Bank for after hours or when the line is busy. The person answering the phone is not a doctor, nurse or midwife. You will be linked with the Mesh Clinic for an appointment if appropriate. Unfortunately there are currently long waiting times for appointments.
- In WA there is the WA Pelvic Mesh Support Group which can connect you with women who have had these procedures
- Take this information sheet to your trusted health provider to discuss your current or future options
What has been done about regulating mesh?
The Therapeutic Goods Administration (TGA) regulates medications and medical devices. However, the evidence required to register a device is by no means as comprehensive as that required to register a medication.
What can I do to report complications?
You can register your complications on The Therapeutic Goods Administration (TGA) website here: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
You can also call the Mesh Line if you are in WA on 1800 962 202
What happened about the Senate Inquiry into mesh?
A Senate Inquiry into pelvic mesh was held in 2017, and the Recommendations have largely been accepted by our nation's Health Minister, who apologised to women harmed by mesh implants. They are currently in the early stages of being implemented, and health consumer councils across Australia are working with key bodies to ensure that there is a more consistent approach across Australia.
What about hernia mesh?
Hernia mesh is emerging as the next key area of interest. The complications are very similar, as is the negative impact on people, and the difficulties they can face in getting help. A new peer group has been started in WA - Mesh Too Western Australia.
International Mesh Awareness Day – 1st May
Monday 1st May is International Mesh Awareness Day, the start of Mesh Awareness month. It highlights the complications suffered by women who have had mesh implants to treat stress urinary incontinence and pelvic organ prolapse.
You may have seen a recent episode on The Project which highlighted the little known reality that when a urogynecological mesh implant goes wrong, it can go badly wrong, with life-changing effects for the women affected. It has taken the recent media activity on the topic for some women to recognise the symptoms in themselves. And despite what Waleed Ally stated in the final moments of the Project episode on the topic, complications can occur quite some time after implanting, and only partial removal options exist for women.
The use of mesh is now the subject of a federal Senate Inquiry, which is taking submissions until the 31st May 2017. The Inquiry’s title “Number of women in Australia who have had transvaginal mesh implants and related matters” highlights that we simply don’t know how many women have had these implants, and how many of them have suffered complications.
Health Issues Centre Victoria hosted a Facebook Page “Understanding pelvic mesh implants and impacts on women in Australia”. This page is part of a united response by health consumers councils across Australia to ensure women’s voices are at the heart of the Senate Inquiry Submission. It links to an anonymous survey where women and their families are able to provide feedback to inform the joint Submission. The page will be active until the Inquiry Submission deadline of 31st May 2017.
Pictured: Caz Chisholm holding both her awards
Here in WA, on Thursday 27th April, the Health Consumers’ Council announced our Health Consumer Excellence Awards. The winner of the Health Consumer Award, and the Rosemary Caithness Award to acknowledge outstanding service to health consumers was the same person – Caz Chisholm. Caz is one of the founders of the Australian Pelvic Mesh Support Group, a Facebook page which has grown from 39 members two years ago to just under 600 members in the last week, after the airing of the Project episode. She has spent significant time and energy raising awareness for women about the issue and providing essential peer support. She was also directly responsible for ensuring that the Senate Inquiry was successfully advocated for by Senator Hinch in the first place.
For women and families affected by pelvic mesh, we urge you to have your say to ensure the consumer voice is central to the Submission. Check the Having A Say section lower down on this page for the links to the different ways to provide your feedback.
Please also note that the health consumers councils across Australia have developed a Consumer Information Sheet which appears below and is also available as a PDF. Please contact us on info@hconc.org.au or 9221 3422 if you have any comments or concerns.
Consumer information
For women who have had, or are considering having surgery to treat stress urinary incontinence and pelvic organ prolapse
If you have been diagnosed with pelvic organ prolapse or stress urinary incontinence, the likelihood is that you will be offered surgery once non-surgical options such as physiotherapy have been exhausted.
Surgery for these two conditions are usually involves a mesh insertion or implant. It might be called tape or a sling. It is all the same from a consumer perspective and these products are collectively known as mesh. The Therapeutic Goods Advisory Website has an updated list of complications associated with surgery using mesh. https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
Mesh implants have been offered to women since the late 1990s. The procedure is considered to be only partially reversible, and some women have travelled to America at their own expense to have mesh removed.
Before you consent to any surgical procedure, it is important to ask all the questions you need so you understand what you are consenting to. The Choosing Wisely campaign has created these questions to help you get started. http://www.choosingwisely.org.au/resources/consumers/5-questions-to-ask-your-doctor
1. Do I really need this test or procedure?
Tests may help you and your doctor or other healthcare provider determine the problem and the procedures that may help to treat it.
2. What are the risks?
Will there be side effects? What are the chances of getting results that aren’t accurate? Could that lead to more testing or another procedure?
3. Are there simpler, safer options?
Sometimes all you need to do is make lifestyle changes, such as eating healthier foods or exercising more. Another option to ask your doctor about is native tissue repair.
4. What happens if I don’t do anything?
Ask if your condition might get worse — or better — if you don’t have the test or procedure right away.
Stress urinary incontinence is not a life-threatening condition so consider carefully before undergoing any surgery. Do not consider surgery until all non-surgical options have been exhausted.
5. What are the costs?
Costs can be financial, emotional or a cost of your time. Where there is a cost to the community, is the cost reasonable or is there a cheaper alternative?
What help can I access?
- There is a Facebook group called the Australian Pelvic Mesh Support Group which can connect you with women who have had these procedures.
- Shine Lawyers is one of the firms that is currently undertaking class actions in relation to mesh
- Take this information sheet to your trusted health provider to discuss your current or future options
Having A Say
- Currently, there is a Senate Inquiry into the use of mesh. It is specifically looking to discover how many women have had a mesh implant, the impact of these implants, what the consent processes were, what removal options are available, what the Therapeutic Goods Administration role has been in it. Women are invited to make a submission to the senate inquiry with their story. http://www.aph.gov.au/Parliamentary_Business/Committees/Senate/Community_Affairs/MeshImplants
- As noted above, Health Issues Centre Victoria is hosting a Facebook Page Understanding pelvic mesh implants and impacts on women in Australia. This page is part of a united response by each state’s health consumers councils across Australia to ensure women’s voices are at the heart of the Senate. The page will be active until the Inquiry Submission deadline of 31st May 2017. Inquiry. https://www.facebook.com/UnderstandingPelvicMesh/
- The Therapeutic Goods Administration is seeking information from members of the public about complications. https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
- The Australian Commission into Safety and Quality in Healthcare is also undertaking work develop guidance for consumers, clinicians and health services on the use of transvaginal mesh products for the treatment of pelvic organ prolapse and stress urinary incontinence. https://www.safetyandquality.gov.au/our-work/transvaginal-mesh/
Complications associated with use of Pelvic Mesh
These are listed on Australia’s Therapeutic Goods Administration (TGA) website as follows: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
|
|
Author: Pip Brennan, Executive Director of the Health Consumers’ Council. Consumer Member on the Australian Commission on Safety and Quality in Health Services Reference Committee.
Archived Systemic Work
Below are summaries of some of the many systemic actions we have been involved in over the past 5 years. On the side menu, you will see our most recent/ongoing systemic projects, partnerships and involvements.
If you have any questions about Systemic Advocacy in the Health System, or about any of our listed involvements, please email info@hconc.org.au
Alcohol & Other Drug Consumer & Community Coalition

Background
In 2015, the Health Consumers’ Council was funded to co-ordinate a project to build on the recommendations from the November 2014 Forum, Improving Consumer Involvement in the Alcohol and Other Drug Sector. An Alcohol and Other Drug Advisory Group (AODAG) comprising government agencies, not for profit organisations and consumers was set up to oversee progress.
The project specifically addressed the following two recommendations:
- to develop a common set of principles for engagement
- outline best practice engagement strategies for the sector
In 2017 the WA Primary Health Alliance funded HCC to support the ongoing work of the Alcohol and Other Drug Advisory Group (AODAG) to oversee a new project entitled “Improving Consumer Involvement in the Alcohol and Other Drug Sector”.
It was agreed that the term ‘alcohol and other drug consumers’ was inclusive of current users, service users, potential service users, family members and supporters.
The Alcohol and Other Drug Consumer & Community Coalition (AODCCC) was incorporated in June 2018 in response to the need and support for an AOD specific consumer advocacy body. We have recently received funding from the Mental Health Commission in order to progress our establishment and have now released our Mission, Vision and Values.
AODCCC Membership
Membership is open to people who use or who have used alcohol and other drugs, their family members and significant others. A link to an online membership application can be found here and on the Facebook page. Hard copy applications are available here and can be emailed to info@aodccc.org.
Management Committee
Full details of the current Management Committee are provided on the Australian Charities and Not-for-profit Commission (ACNC) website.
Contact AODCCC
For any information please contact:
Email info@aodccc.org
Phone (08) 6311 8402
Cancer Care
Cancer Care
The Cancer Plan was released in February 2020 setting out the next five years of strategy in relation to cancer services. This work was undertaken by the WA Department of Health, and the Health Consumers’ Council supported the project through running a community survey and developing consumer videos reflecting consumer patient journey experiences. A summary of survey results is available here. The launch event featured a moving and articulate presentation from Advisory Group member Susannah Morris, who ensured the consumer voice was at the heart of the plan as much as possible.
Cancer Research
In May 2019 the Health Department’s Health Research Future Fund sought feedback on the involvement of consumers in cancer research. A large forum was convened with researchers and clinicians across the sector. HCC was funded to enhance the consumer voice into the process. We undertook a consumer survey, and presented a short video with consumer and carer experiences of being involved in research. Click the link for the Consumer insights in Medical Research Cancer PowerPoint.
In summary, we strongly agree with the National Health and Medical Research Council that:
“Consumer and community involvement is about research being carried out with or by consumers and community members rather than to, about or for them.”
The Cost of Cancer Care
The Health Consumers’ Council partnered with Cancer Council WA to find out whether people are making informed financial decisions about where to get their cancer care.
We developed a short survey to find out more about the issue, and a report of the findings is here.
Dental Care
Dental Care
Access and costs are two issues we hear about frequently from consumers when it comes to dental care.
We have previously held a seat on the State Oral Health Advisory Committee; spoken on the radio with Geoff Hutchison about a consumer’s costs related to a child’s wisdom teeth; and run a survey to gather consumer stories and views on dental health. In 2023 we promoted a survey to encourage consumers to share their experiences as part of the Senate Select Committee into the Provision of and Access to Dental Services in Australia.
Digital Health & My Health Record FAQs
Digital Health
Our work in the digital health space is ongoing. Below is an archive of some of the previous work we have been involved.
There is so much going on in the digital health space. It is a complex area and difficult to know what issues need to focus on. People are rightly concerned about their data and its privacy. But being able to share your health information quickly could mean the difference between life and death. Queensland Health developed a Consumer Charter on Digital Health which aims to reflect consumer priorities and needs in relation to digital health.
In WA the Digital Health Strategy 2020-2030 was released, and a key initial deliverable will be creating a statewide electronic medical record in our hospitals. This may seem confusing, given that the My Health Record was implemented nationwide in 2019. As at December 2019, 22.68 million Australians had a My Health Record, with 2.4 million of those in WA. (See here) A key thing to remember is that:
- An electronic health record is designed to have a more overall view of someone’s health, across hospitals, GPs, pharmacists etc.
- A medical health record tracks medical care usually within one hospital.
We are currently working with the WA Department of Health to develop a Consumer Charter which focuses on digital health. HCC are convening 10 Kitchen Table Discussions on the topic and is currently seeking Discussion Hosts. The Kitchen Table Discussion comments will be used to form a Consumer Charter – this will include non-negotiable principles to guide future direction.
My Health Record Resources
In 2019, the Australian Digital Health Agency released a number of new resources, and we partnered with them to share them on our website and through social media. We also undertook a Consumer Survey – you can find the full report of our work here.
If you are using My Health Record, we recommenced you log in to take a look at your information and update your privacy settings. These brochures provide further information on how to use your My Health Record now that it has been set up.
- Your Health Information securely in one place (general information on how your health records are stored)
- Control who can look at your health information (includes how to set privacy controls)
- How is your health information protected (more information on privacy and security)
How can I find out more?
Check out these Frequently Asked Questions
Please email us if you have any concerns regarding the My Health Record and we will ensure you are given access to the information you need.
Empowering Consumers with Disabilities
- Empowering Health Consumers with Disabilities – Resource List
- WA Getting Ready to Go Home (NDS project to improve the transition experience for people with a disability from hospital to community)
HCC partnered with People With disabilities WA to deliver a project which examined health literacy materials and put them to the test of disability friendliness. The project delivered nine training sessions on Disability Health Rights for people with disabilities, and their carers, family and support people. Topics covered included: rights, ideas for getting better care, where to go for help, medical records and information sharing, and navigating the health system.
A series of booklets and videos were produced for this project, and are linked below. Working group members also shared their views on how health services could engage more with people with disabilities at this blog article:
Plain English
- Better Healthcare for People with Disabilities – PE
- Better Hospital Care for People with Disabilities – PE
Easy-read
- Better Healthcare for People with Disabilities – ER
- Better Hospital Care for People with Disabilities – ER
Plain-text (screen-reader compatible)
- Better Healthcare for People with Disabilities – PT
- Better Hospital Care for People with Disabilities – PT
Videos
Feedback Processes
In 2020, Health Consumers’ Council (HCC) worked with the Patient Safety Surveillance Unit in the Department of Health to learn more about how consumer feedback – including complaints and compliments – is collected, provided, and used for improving health services. We held a number of workshops with consumers and we also held telephone interviews with some consumers in regional areas. We held targeted sessions for Aboriginal community members, and Consumers of Mental Health WA ran a targeted session for consumer of mental health services.
Click to see issues, barriers and ideals from this consultation
Care Opinion
In 2020 the Patient Opinion platform, an independent, moderated place for people to provide feedback, was renamed to Care Opinion. This platform is now one portal for people to provide feedback on health and social services. It mirrors the same platform available in the UK, which uses the power of story to transform health and human services.
A non-profit organisation moderates the platform, and services subscribe to be able to receive notifications, reports etc. WA is the first state to have every public hospital as a subscriber. You can find out more or post a story here.
WA Health Complaint Policy Review
The Department of Health (DoH) consulted on a revised version of the WA Complaints Management Policy and these new versions appear below. We undertook a series of consultations to support the work survey and have collated this feedback.
- Updated Complaints Management Policy – main draft policy – this is mandatory for WA Health services
- Updated Complaints Management Guideline – supporting document to expand on how the implementation of the policy – non-mandatory
- Updated Complaints Management Toolkit – supporting document including suggested templates for letters and forms – non-mandatory
WA Health Review of the complaints and feedback process
Following on from this consultation and the release of the new complaints guidelines, DoH consulted about the process of making a complaint and giving feedback. We heard about the many barriers to giving feedback, including concerns about what might happen to the feedback. This was especially prominent in the discussions we had with Aboriginal people. It was also raised that there is no easy way to give feedback about the whole system, not just one health service.
Informing New Models of Primary Care 2017
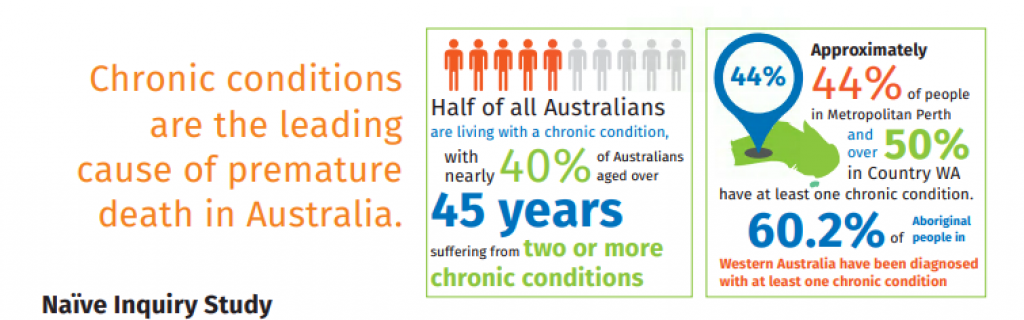 Informing New Models of Primary Care was a 6 month collaborative project between the WA Primary Health Network (WAPHA), Health Consumers’ Council, and Curtin University undertaken in 2017. Primary Care refers to the care you receive from your GP and other health care providers outside of the hospital system. WAPHA is supported by funding from the Australian Government under the nation’s Primary Health Network Program.
Informing New Models of Primary Care was a 6 month collaborative project between the WA Primary Health Network (WAPHA), Health Consumers’ Council, and Curtin University undertaken in 2017. Primary Care refers to the care you receive from your GP and other health care providers outside of the hospital system. WAPHA is supported by funding from the Australian Government under the nation’s Primary Health Network Program.
Prior to this project being established, WAPHA and Curtin undertook consultations with general practice staff to inform how care can best be provided to people to keep them well and out of hospital as much as possible.
Informing New Models of Primary Care project was the second stage, and HCC worked with WAPHA and Curtin but this time focusing on the experience of people who access GP services. It involved convening a series of focus groups with people with multiple chronic health conditions with management under a Care Plan. Findings of these discussions have been compiled in the Naive Inquiry Brochure and were shared with the community at a community forum held on 1st December 2017. This forum provided an opportunity to further the conversation on the developing models of care.
Medical Devices
Have you seen the Netflix Documentary The Bleeding Edge? In not, watch it now…
The day before the National Mesh Forum, which was convened on 5th April 2019 by the Health Consumers Councils across Australia and funded by state health departments, the Therapeutic Goods Administration (TGA) released Action Plan for Medical Devices. This was discussed at the Forum and is the culmination of some months work, but health consumers councils were not included in its development.
Strategies on the Plan:
Strategy 1
Improve how new devices get on the market
Strategy 2
Strengthen monitoring and follow-up of devices already in use
Strategy 3
Provide more information to patients about the devices they use
If there’s one thing consumers need to know…
Devices do not need to have as much evidence behind them as medications in order to be listed with the TGA. This is in part reflects the assumption that there is a detailed consent conversation between patients and their surgeons. We would urge all people to think of any procedure requiring any implanted medical device as an experimental treatment, and consent with that level of attention and care.
In essence, medical device companies assure TGA of the safety of their devices. It is a highly competitive and lucrative market, every bit as powerful as pharma, or perhaps more so. Post-market testing is supposed to occur, noting when complications occur and ensuring the TGA are aware. This doesn’t happen as much as it needs to, and is not compulsory for surgeons, although it is for medical device companies. Technically the TGA can prosecute medical device companies who don’t advise of complications but in practice this happens rarely.
Again, we recommend you watch the Bleeding Edge Documentary to understand more and what’s at stake for patient safety.
Bleeding Edge Documentary
America has the most technologically advanced health care system in the world, yet medical interventions have become the third leading cause of death, and the overwhelming majority of high-risk implanted devices never require a single clinical trial.
In The Bleeding Edge, Academy Award nominated filmmakers Kirby Dick and Amy Ziering (The Invisible War, The Hunting Ground) turn their sights on the $400 billion medical device industry, examining lax regulations, corporate cover-ups, and profit driven incentives that put patients at risk daily.
Across the globe there is an investigation underway by the International Consortium of Investigative Journalists about how medical devices are listed on the different jurisdiction’s list of approved devices. Called The Implant Files, the Consortium’s website provides latest news and updates in relation to implants.
The Health Consumers’ Council in WA recently noted the implications for how devices are put onto our Therapeutic Goods Administration (TGA) list through the work done on the Pelvic Mesh Inquiry held in 2017-18. In summary, the TGA often relies on slim evidence from other jurisdictions to approve a device, and whether there are any reports of post implant complications to confirm a device’s safety. However, reporting complications is not compulsory, and very often, clinicians don’t. They may not be aware that there is a trend, thinking “it’s only this one person, so is it relevant?” or for whatever reason, they don’t report. Consumers can report faults in implants they have had put into their body, if they know there is a place to do so on the TGA website, and if they know the serial number of the device. In other words, this is also not likely.
There is no easy way of knowing which human being has which implant, as there are only registers for certain kinds of devices, and records are often not digitised or easily shareable for it to be easy to do a product recall. It should be like doing an airbag recall for your car, but it isn’t.
The Health Issues Centre in Victoria has begun an anonymous survey for consumers who think they may have been impacted by implants, which you can complete by clicking on this link. Hernia mesh has already emerged as one of the leading implants causing pain and suffering for patients.
Mesh Implants
A GLOBAL HEALTH CRISIS – PELVIC MESH IMPLANTS
It has taken some time for the scale and extent of the impact of pelvic mesh implants for women to treat stress urinary incontinence and pelvic organ prolapse. Once hailed as the perfect solution for an enduring surgical fix for these non-life-threatening conditions, it has left a swathe of women with permanent, life altering consequences. Persistent pelvic pain at rest. Inability to have sex. Inability to continue working, and the financial impact often amplified by failed marriages as the lack of intimacy took its toll. The full list of complications is listed on the Therapeutic Goods Administration mesh hub.
In 2017 Australia undertook a Senate Inquiry – entitled Number of women in Australia who have had transvaginal mesh implants and related matters. We literally did not know how many women had been impacted. There were 13 recommendations in the final report, with a mix of federal and state responsibilities to effect implementation. There was even one on effective informed consent processes. It was clear from submissions and hearings that women were not informed about the potential horrific consequences of their choice, and that the mesh is extremely complex to remove. With the divide of responsibility between state and federal governments and the fact that most of the implant surgeries were performed in private hospitals, it is difficult to track real progress. Some meshes have been banned from use, but by no means all. Many women are still unaware that their sequelae of symptoms are related to their mesh implants. GPs and specialists may also be unaware.
WA PELVIC MESH SUPPORT GROUP
The peer support group the WA Pelvic Mesh Support Group has its own website and is an essential stakeholder in WA’s response to the mesh crisis.
WA PELVIC MESH COMPLICATIONS CLINIC
This clinic has been set up in King Edward Memorial Hospital and has been operating since 2017. There is a committee of clinicians and consumers who meet to discuss the clinic’s model and progress, as this area is complex and changing. The committee continues to aim to advance the recommendations of the Inquiry.
UNFINISHED BUSINESS – A NATIONAL FORUM ON THE IMPACT OF MESH IMPLANTS
 A National Mesh Implant Forum was held in Melbourne on Friday April 5, 2019, to consider all aspects of Australia’s mesh implant crisis. The Forum was proudly convened by the Health Issues Centre and Health Consumers NSW, Health Consumers Queensland, Health Consumers’ Council (WA), Health Consumers Alliance of South Australia, Health Care Consumers (ACT), Health Consumers Tasmania.
A National Mesh Implant Forum was held in Melbourne on Friday April 5, 2019, to consider all aspects of Australia’s mesh implant crisis. The Forum was proudly convened by the Health Issues Centre and Health Consumers NSW, Health Consumers Queensland, Health Consumers’ Council (WA), Health Consumers Alliance of South Australia, Health Care Consumers (ACT), Health Consumers Tasmania.
The event brought together mesh injured consumers, carers, regulatory authorities, health officials, the Chair of the Senate Inquiry into mesh and consumer advocates to create solutions and bring about real change. The forum considered not only the impact of pelvic mesh, but the emerging parallel crisis involving people who have received hernia mesh implants. A full report is available here.
NEW REPORT – HERNIA MESH IMPLANTS – CONSUMER SURVEY
Health Issues Centre Victoria initiated the Mesh Device and Implant Failure study late last year and of the respondents, a sizeable 183 patients have already reported major problems with their hernia mesh implants. 70 per cent of these are men. You can read the report here.
According to publicly available figures nearly 100,000 Australians are hospitalised for hernia each year. However, the numbers of patients that go on to have pelvic mesh implants and that are negatively impacted is not known. People who would like to report complications of hernia procedures using mesh can complete the survey here.
PELVIC MESH FAQs
What is pelvic mesh?Pelvic Mesh refers to polypropylene mesh implants to treat women treated for stress urinary incontinence or pelvic organ prolapse.
What are the complications of pelvic mesh?Complications include pain, inflammatary reactions to the mesh, persistent infections, bleeding, with the mesh kinking, moving or migrating and causing damage to surrounding organs.
The actual number of women who experience complications may be under-reported, so while some women experience the benefits from implants, other women experience any or all of these complications as they are listed below from Australia’s Therapeutic Goods Administration (TGA) website: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
-punctures or lacerations of vessels, nerves, structures or organs, including the bladder, urethra or bowel (these may require surgical repair
-transitory local irritation at the wound site
-a ‘foreign body response’ (wound breakdown, extrusion, erosion, exposure, fistula formation and/or inflammation)
-mesh extrusion, exposure, or erosion into the vagina or other structures or organs
-as with all foreign bodies, mesh may potentiate an existing infection
-over-correction (too much tension applied to the tape) may cause temporary or permanent lower urinary tract obstruction
-acute and/or chronic pain
-voiding dysfunction
-pain during intercourse
-neuromuscular problems including acute and/or chronic pain in the groin, thigh, leg, pelvic and/or abdominal area
-recurrence of incontinence
-bleeding including haemorrhage, or haematoma
-seroma
-urge incontinence
-urinary frequency
-urinary retention
-adhesion formation
-atypical vaginal discharge
-exposed mesh may cause pain or discomfort to the patient’s partner during intercourse
-mesh migration
-allergic reaction
-abscess
-swelling around the wound site
-recurrent prolapse
-contracture
-scarring
-excessive contraction or shrinkage of the tissue surrounding the mesh
-vaginal scarring, tightening and/or shortening
-constipation/defecation dysfunction
-granulation tissue formation.
I've been told that it is a new type of mesh, or that it's a sling. Is this the same?Mesh, tape, sling - it is all polypropylene mesh. It is a complex area and rapidly changing so clinicians may not be aware that they are in essence, all the same. If you don't want mesh, you have the right to request native tissue repair or a procedure like a Burch colposuspension. It is your body and you need to feel confident you are providing informed consent.
What are the alternatives to using mesh for incontinence and prolapse?Non-surgical options includes physiotherapy and pessaries. Surgery should be considered a last resort when all other options have been exhausted.
There are surgical options which don't include mesh such as Native Tissue Repair and Burch Colposuspension. Have a look at the Australian Commission on Safety and Quality in Healthcare's resources on this page for Pelvic Organ Prolapse and Stress Urinary Incontinence and remember the key advice that surgery should be the last resort when all other options have been exhausted.
You will be the one who will bear the consequences if you do have complications from the mesh, so it's important that you provide informed consent. The Choosing Wisely campaign has created these questions to help you get started. http://www.choosingwisely.org.au/resources/consumers/5-questions-to-ask-your-doctor - plus it is useful to ask how many of the same procedures your surgeon has done, and what the outcomes have been. Any reluctance to answer this question may signal you have not found the right surgeon for you.
Is mesh banned?No it is not banned. It has been banned for some, but not all types of pelvic organ prolapse surgery, but for the most common surgery, stress urinary incontinence, it has not been banned. From 1 December 2018, all new surgical mesh devices seeking approval from the TGA will need to meet the higher evidentiary requirements of a Class III medical device. This does not apply to mesh devices already on the TGA register however.
Can I get the mesh taken out?It is very difficult to fully remove mesh. Women are offered partial removals of mesh, for example snipping of the part protruding through the vaginal wall. Many women do not want partial removals as the remaining mesh frays and causes ongoing issues, and it may be more difficult to get the rest of the mesh out. Some women have taken the decision to self-fund and travel overseas to where other surgeons more experienced in full mesh removal may be able to provide assistance. We are continuing to work on this as a nation and the options are continually evolving. The WA Pelvic Mesh Support Group can be an important source of support to find out latest options, or you can call the Health Consumers Council on 9221 3422/ 1800 620 780 for country callers, or email info@hconc.org.au
What help is available for women?- You can call the WA Pelvic Mesh Clinic line at King Edward Hospital on 1800 962 202. This is answered from 8.30-4pm Monday to Friday, with a Message Bank for after hours or when the line is busy. The person answering the phone is not a doctor, nurse or midwife. You will be linked with the Mesh Clinic for an appointment if appropriate. Unfortunately there are currently long waiting times for appointments.
- In WA there is the WA Pelvic Mesh Support Group which can connect you with women who have had these procedures
- Take this information sheet to your trusted health provider to discuss your current or future options
What has been done about regulating mesh?The Therapeutic Goods Administration (TGA) regulates medications and medical devices. However, the evidence required to register a device is by no means as comprehensive as that required to register a medication.
What can I do to report complications?You can register your complications on The Therapeutic Goods Administration (TGA) website here: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
You can also call the Mesh Line if you are in WA on 1800 962 202
What happened about the Senate Inquiry into mesh?A Senate Inquiry into pelvic mesh was held in 2017, and the Recommendations have largely been accepted by our nation's Health Minister, who apologised to women harmed by mesh implants. They are currently in the early stages of being implemented, and health consumer councils across Australia are working with key bodies to ensure that there is a more consistent approach across Australia.
What about hernia mesh?Hernia mesh is emerging as the next key area of interest. The complications are very similar, as is the negative impact on people, and the difficulties they can face in getting help. A new peer group has been started in WA - Mesh Too Western Australia.
What is pelvic mesh?
Pelvic Mesh refers to polypropylene mesh implants to treat women treated for stress urinary incontinence or pelvic organ prolapse.
What are the complications of pelvic mesh?
Complications include pain, inflammatary reactions to the mesh, persistent infections, bleeding, with the mesh kinking, moving or migrating and causing damage to surrounding organs.
The actual number of women who experience complications may be under-reported, so while some women experience the benefits from implants, other women experience any or all of these complications as they are listed below from Australia’s Therapeutic Goods Administration (TGA) website: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
-punctures or lacerations of vessels, nerves, structures or organs, including the bladder, urethra or bowel (these may require surgical repair
-transitory local irritation at the wound site
-a ‘foreign body response’ (wound breakdown, extrusion, erosion, exposure, fistula formation and/or inflammation)
-mesh extrusion, exposure, or erosion into the vagina or other structures or organs
-as with all foreign bodies, mesh may potentiate an existing infection
-over-correction (too much tension applied to the tape) may cause temporary or permanent lower urinary tract obstruction
-acute and/or chronic pain
-voiding dysfunction
-pain during intercourse
-neuromuscular problems including acute and/or chronic pain in the groin, thigh, leg, pelvic and/or abdominal area
-recurrence of incontinence
-bleeding including haemorrhage, or haematoma
-seroma
-urge incontinence
-urinary frequency
-urinary retention
-adhesion formation
-atypical vaginal discharge
-exposed mesh may cause pain or discomfort to the patient’s partner during intercourse
-mesh migration
-allergic reaction
-abscess
-swelling around the wound site
-recurrent prolapse
-contracture
-scarring
-excessive contraction or shrinkage of the tissue surrounding the mesh
-vaginal scarring, tightening and/or shortening
-constipation/defecation dysfunction
-granulation tissue formation.
I've been told that it is a new type of mesh, or that it's a sling. Is this the same?
Mesh, tape, sling - it is all polypropylene mesh. It is a complex area and rapidly changing so clinicians may not be aware that they are in essence, all the same. If you don't want mesh, you have the right to request native tissue repair or a procedure like a Burch colposuspension. It is your body and you need to feel confident you are providing informed consent.
What are the alternatives to using mesh for incontinence and prolapse?
Non-surgical options includes physiotherapy and pessaries. Surgery should be considered a last resort when all other options have been exhausted.
There are surgical options which don't include mesh such as Native Tissue Repair and Burch Colposuspension. Have a look at the Australian Commission on Safety and Quality in Healthcare's resources on this page for Pelvic Organ Prolapse and Stress Urinary Incontinence and remember the key advice that surgery should be the last resort when all other options have been exhausted.
You will be the one who will bear the consequences if you do have complications from the mesh, so it's important that you provide informed consent. The Choosing Wisely campaign has created these questions to help you get started. http://www.choosingwisely.org.au/resources/consumers/5-questions-to-ask-your-doctor - plus it is useful to ask how many of the same procedures your surgeon has done, and what the outcomes have been. Any reluctance to answer this question may signal you have not found the right surgeon for you.
Is mesh banned?
No it is not banned. It has been banned for some, but not all types of pelvic organ prolapse surgery, but for the most common surgery, stress urinary incontinence, it has not been banned. From 1 December 2018, all new surgical mesh devices seeking approval from the TGA will need to meet the higher evidentiary requirements of a Class III medical device. This does not apply to mesh devices already on the TGA register however.
Can I get the mesh taken out?
It is very difficult to fully remove mesh. Women are offered partial removals of mesh, for example snipping of the part protruding through the vaginal wall. Many women do not want partial removals as the remaining mesh frays and causes ongoing issues, and it may be more difficult to get the rest of the mesh out. Some women have taken the decision to self-fund and travel overseas to where other surgeons more experienced in full mesh removal may be able to provide assistance. We are continuing to work on this as a nation and the options are continually evolving. The WA Pelvic Mesh Support Group can be an important source of support to find out latest options, or you can call the Health Consumers Council on 9221 3422/ 1800 620 780 for country callers, or email info@hconc.org.au
What help is available for women?
- You can call the WA Pelvic Mesh Clinic line at King Edward Hospital on 1800 962 202. This is answered from 8.30-4pm Monday to Friday, with a Message Bank for after hours or when the line is busy. The person answering the phone is not a doctor, nurse or midwife. You will be linked with the Mesh Clinic for an appointment if appropriate. Unfortunately there are currently long waiting times for appointments.
- In WA there is the WA Pelvic Mesh Support Group which can connect you with women who have had these procedures
- Take this information sheet to your trusted health provider to discuss your current or future options
What has been done about regulating mesh?
The Therapeutic Goods Administration (TGA) regulates medications and medical devices. However, the evidence required to register a device is by no means as comprehensive as that required to register a medication.
What can I do to report complications?
You can register your complications on The Therapeutic Goods Administration (TGA) website here: https://www.tga.gov.au/alert/urogynaecological-surgical-mesh-complications
You can also call the Mesh Line if you are in WA on 1800 962 202
What happened about the Senate Inquiry into mesh?
A Senate Inquiry into pelvic mesh was held in 2017, and the Recommendations have largely been accepted by our nation's Health Minister, who apologised to women harmed by mesh implants. They are currently in the early stages of being implemented, and health consumer councils across Australia are working with key bodies to ensure that there is a more consistent approach across Australia.
What about hernia mesh?
Hernia mesh is emerging as the next key area of interest. The complications are very similar, as is the negative impact on people, and the difficulties they can face in getting help. A new peer group has been started in WA - Mesh Too Western Australia.
Pregnancy and Maternity Care
My Baby WA Pregnancy App
The My Baby WA app launched in June 2021 withy a massive initial response.
The app was developed through a partnership between the WA Country Health Service and Health Consumers’ Council Wa. The app is to assist women and families to navigate the pregnancy, birth and early parenting periods- providing information that is specific for women and families in Western Australia.
My Baby WA provides pregnant women and families in Western Australia accessible and evidence based information during their pregnancy. Functions on the app include;
· All the information you need on pregnancy, birth and your baby
· A WA maternity service locator including models of care available at each service
· Week by week pregnancy information
· An interactive timeline for women to track their appointments, tests, screening and education offered to them during their pregnancy
· A baby bump photo gallery
· Noongar lullabies to play and sing to your unborn baby
· Option to fill in the Women’s Experiences of Maternity Services to Survey to provide feedback to you maternity service.
· Mum and Partner modes for pregnancy, birth and early parenting tips
The app can be downloaded on iPhone or Android.
International Patient Safety Day Q&A Panel – Maternal and newborn safety
To mark World Patient Safety Day 2021, and the theme of safe maternal and newborn care, in partnership with AHPRA and Women’s and Newborns Health Network, Health Consumers’ Council convened a Q&A panel discussion exploring maternal and childbirth care.
We explored topics such as Aboriginal women’s experiences of childbirth, the impact of COVID on birthing women, why women and families’ feedback is important and how it changes things. We also confirmed the importance of education, and of involving birthing women and families at all stages and at all levels in designing and evaluating maternity services.
Listen on catch-up (1.5 hours)
National Strategic Approach to Maternity Services
We have been involved with this national strategy as much as possible, although it has been some time since there was an update. You can find out more about maternity services in Australia here.
Media releases
Please find below statements released by Health Consumers’ Council.
We welcome contact from journalists on health and health consumer topics and are happy to provide information, interviews and quotes.
For media requests, please contact:
Executive Director | Clare.Mullen@hconc.org.au | 0488 701 839
or Marketing & Communications | TA.Fyson@hconc.org.au
18/03/25 Health Consumers’ Council welcomes new WA ministerial health team
17/11/23 Health Consumers’ Council WA welcomes increased COVID-19 health protections in hospitals
Health Consumers’ Council welcomes the return of COVID-19 health protections in hospitals as COVID-19 infections rise. We can all play a part in a healthy WA.
31/08/23 HCC welcomes mental health reforms
Health Consumers’ Council welcomes the State Government’s decision to elevate the voice of people with lived experience and consumers in how mental health services are designed, developed and overseen. We commend the Government’s decision to listen to people with lived experience, consumer advocates and others to retain current governance structures with a renewed focus on culture change, accountability and strong lived experience voices.
29/08/2022 Seeking multicultural cancer patients and carers to improve cancer information resources
For State-wide, regional and rural WA especially, and men: Community consultations on the cancer information needs of culturally and linguistically diverse (CaLD) consumers and carers will be held for men, particularly 1st September, and all regional multicultural people 13th September 2022. There are no cancer resources or publications specifically for culturally and linguistically diverse (CaLD) patients or carers for Western Australian regional communities, men specifically. A consultation discussion project aims to start the process to change that. Health Consumers’ Council (HCC) WA is seeking multicultural, ethnically and linguistically diverse people in the State’s regional and rural areas, and men in particular across metro Perth, to discuss cancer information needs. HCC is specifically looking for CaLD people who have or had cancer – patients – or who are caring for, or cared for, a loved one with cancer to participate in discussions. Contact Nadeen@hconc.org.au /read more…
26/07/2021 Health Consumers’ Council joins The Great Registration Race for DonateLife Week
Health Consumers’ Council has received a 2021 Community Awareness Grant from the Organ and Tissue Authority to undertake a project aimed at empowering Western Australians to increase their knowledge of the benefits of organ and tissue donation and transplantation, to encourage family discussion and know each other’s donation decisions, and to register online on the Australian Organ Donor Register.
27/11/2020 It’s time to change the way we speak about obesity
Health Consumers’ Council welcomes a new media and communications guide changing the narrative around obesity. Shift. A guide for media and communications professionals is a new communications tool that aims to work with media to influence better public perceptions of overweight and obesity.
29/11/2019 Duty of Care or Buyer Beware? TGA resonse to Shine class action decision
Despite the TGA’s most recent media release claiming progress in the battle for a just resolution to the pelvic mesh crisis, little has changed since the Senate Inquiry into Pelvic Mesh handed down its recommendations in 2018. Peak state Health consumer bodies spell out what still needs to be done.
22/11/2019 Vindicated! But justice deferred – Shine class action against Johnson & Johnson
Peak state Health Consumer bodies have welcomed the judgement vindicating the more than 1200 mesh injured women who participated in the Shine class action against Johnson & Johnson but reserved judgement on the outcome until the size of the final settlement is announced.
1/05/2019 Health Consumer Excellence Award winners announced
Health Consumers’ Council (HCC) has honoured the everyday heroes in health with the annual Health Consumer Excellence Awards
10/04/2019 Health Consumers’ Council welcomes the Sustainable Health Review Final Report
Health Consumers’ Council (WA) Executive Director Pip Brennan welcomed the report and its recommendations, and said HCC was looking forward to working together with health staff, consumers, non-profit organisations, and the community at large to bring the strategies into action.
11/03/2019 Heritage Identification study published by the Medical Journal of Australia
As the peak advocacy body for patients’ rights in WA, Health Consumers’ Council was consulted during the study which formally documented the frequency of references to a patient’s cultural heritage during medical handover and in hospital medical records.
Medical Devices
 Have you seen the Netflix Documentary The Bleeding Edge? In not, watch it now… The day before the National Mesh Forum, which was convened on 5th April 2019 by the Health Consumers Councils across Australia and funded by state health departments, the Therapeutic Goods Administration (TGA) released Action Plan for Medical Devices. This was discussed at the Forum and is the culmination of some months work, but health consumers councils were not included in its development. Strategies on the Plan:
Have you seen the Netflix Documentary The Bleeding Edge? In not, watch it now… The day before the National Mesh Forum, which was convened on 5th April 2019 by the Health Consumers Councils across Australia and funded by state health departments, the Therapeutic Goods Administration (TGA) released Action Plan for Medical Devices. This was discussed at the Forum and is the culmination of some months work, but health consumers councils were not included in its development. Strategies on the Plan:Strategy 1 Improve how new devices get on the market Strategy 2 Strengthen monitoring and follow-up of devices already in use Strategy 3 Provide more information to patients about the devices they use
If there’s one thing consumers need to know…
Devices do not need to have as much evidence behind them as medications in order to be listed with the TGA. This is in part reflects the assumption that there is a detailed consent conversation between patients and their surgeons. We would urge all people to think of any procedure requiring any implanted medical device as an experimental treatment, and consent with that level of attention and care. In essence, medical device companies assure TGA of the safety of their devices. It is a highly competitive and lucrative market, every bit as powerful as pharma, or perhaps more so. Post-market testing is supposed to occur, noting when complications occur and ensuring the TGA are aware. This doesn’t happen as much as it needs to, and is not compulsory for surgeons, although it is for medical device companies. Technically the TGA can prosecute medical device companies who don’t advise of complications but in practice this happens rarely. Again, we recommend you watch the Bleeding Edge Documentary to understand more and what’s at stake for patient safety.Bleeding Edge Documentary
America has the most technologically advanced health care system in the world, yet medical interventions have become the third leading cause of death, and the overwhelming majority of high-risk implanted devices never require a single clinical trial. In The Bleeding Edge, Academy Award nominated filmmakers Kirby Dick and Amy Ziering (The Invisible War, The Hunting Ground) turn their sights on the $400 billion medical device industry, examining lax regulations, corporate cover-ups, and profit driven incentives that put patients at risk daily. Across the globe there is an investigation underway by the International Consortium of Investigative Journalists about how medical devices are listed on the different jurisdiction’s list of approved devices. Called The Implant Files, the Consortium’s website provides latest news and updates in relation to implants. The Health Consumers’ Council in WA recently noted the implications for how devices are put onto our Therapeutic Goods Administration (TGA) list through the work done on the Pelvic Mesh Inquiry held in 2017-18. In summary, the TGA often relies on slim evidence from other jurisdictions to approve a device, and whether there are any reports of post implant complications to confirm a device’s safety. However, reporting complications is not compulsory, and very often, clinicians don’t. They may not be aware that there is a trend, thinking “it’s only this one person, so is it relevant?” or for whatever reason, they don’t report. Consumers can report faults in implants they have had put into their body, if they know there is a place to do so on the TGA website, and if they know the serial number of the device. In other words, this is also not likely. There is no easy way of knowing which human being has which implant, as there are only registers for certain kinds of devices, and records are often not digitised or easily shareable for it to be easy to do a product recall. It should be like doing an airbag recall for your car, but it isn’t. The Health Issues Centre in Victoria has begun an anonymous survey for consumers who think they may have been impacted by implants, which you can complete by clicking on this link. Hernia mesh has already emerged as one of the leading implants causing pain and suffering for patients. This issue of harm through implants is only growing in magnitude, and it is clear we need to overhaul of how we approve devices, and have a clear register of any high risk implant being put into a human body. There needs to be a clearer path for consumers to have the side effects of implants taken seriously, and a much more robust way of providing consent in the first place. This issue will be a focus for us in 2019.Consumer Leaflet Feedback
Click here to read the draft Consumer Information on Mesh Complications
This draft leaflet has been produced by the Australian Commission of Safety and Quality in Health Services. What do you think?
Click here to take the short survey.
This survey has just one question to ask you to rate the leaflet and offering an opportunity to provide a comment.
Click here to take the DISCERN survey
This survey will take at least 15 minutes and uses a validated survey tool to review consumer information, called DISCERN. Organisations are authorised to reproduce The DISCERN Instrument without permission, provided it is used in accordance with the instructions contained in this website to ensure that its methodology is uniform. There are 16 questions over three sections: Reliability, Quality of information on choices, and Overall Rating.
The deadline for all feedback is 8th October. Please contact Pip Brennan pip.brennan@hconc.org.au or 08 9221 3422 if you have any questions.
Rosemary Caithness Award 2017
Rosemary Caithness Award
This award is to acknowledge outstanding service to health consumers. This award is highly selective and typically the recipient has supported health consumers over many years. The Health Consumers’ Council will only award the Rosemary Caithness Award should there be a worthy recipient in any given year.
And the Winner is…
Pictured from left to right: Pip Brennan, Hon. Alanna Clohesy, Carolyn Chisholm and Robyn Nolan.
Carolyn Chisholm
In 2014 Carolyn Chisholm had a transvaginal mesh implant procedure for stress incontinence. She suffered severe pain and an autoimmune reaction from the device that changed her life forever. After discovering at the time these devices could not be fully removed in Australia, Carolyn flew to the USA to have it removed. When she returned, she created a support group for women who are permanently injured by transvaginal mesh devices. The support group has helped many women understand that their symptoms are mesh related, because complications are not widely recognised by doctors and gynaecologists. Carolyn has written to senators, RANZCOG, the Therapeutic Goods Administration and media for over two years. This led her to Senator Derryn Hinch who took on her cause and secured a senate inquiry into transvaginal mesh. Carolyn’s ultimate goal is to have transvaginal mesh banned in Australia because the injuries can be catastrophic and many women will never recover.
Highly Commended is…
Pictured from left to right: Hon. Alanna Clohesy MLA, Robyn Nolan and Jan Thair.
Janice (Jan) Thair
Janice Thair moved from Karrinyup down to the Rockingham area in 1985. From 1989 – 1994 she instigated the formation of Rockingham Women’s Health now called South Coastal Women’s Health.
Janice was also on the Fremantle Hospital Board from 1994 to 1996 and in 2002, she became involved in lobbying to get the local hospital redeveloped (Rockingham General Hospital) and the joined the fledgling Community Advisory Council (CAC).
During this time, Janice set up the ‘Friends of the Hospital’. She is proud of the wonderful concierge service the volunteers still supply today, including the other great services the Friends of the Hospital render to the community.
Janice has been involved with the CAC for 15 years. She has seen the Rockingham District Hospital grow to the fantastic General Hospital it is today, Janice loves that she has been able to serve her community.
Finalists are…
Dr Alex Main
Alex has been contributing to the support of health consumers and carers for 30 years. He has provided pro bono training and consultancy to a range of non-government agencies, and has been a strong lobbyist for improved mental health services in WA. He has been an active member of the boards of various migrant resource centres, of the former Women’s Refuges Multicultural Service, of Relationship Australia, and most recently (with a special mental health portfolio) of Uniting Care West. He was Chairman of AseTTS for many years, and, after formal retirement, he spent 8 years as a pro bono counsellor and therapist with that organisation.
He is one of the instigators of the Let’s Talk Culture series which brings together mental health consumers, carers and practitioners. Currently he is involved in developing training units on migrant and refugee mental health for general practitioners. He continues an active research career in mental health, in his capacity as an Honorary Fellow of Murdoch University.
Health Consumer Award 2017
Health Consumer Award
This award is for health consumers demonstrating excellence in contributing to the improvement of the patient experience. It recognises a health consumer who demonstrates commitment to improving health outcomes and/or the patient experience.
And the Winner is…
Pictured from left to right: Pip Brennan, Hon. Alanna Clohesy MLA, Carolyn Chisholm and Jason Wolf.
Carolyn Chisholm
In 2014 Carolyn Chisholm had a transvaginal mesh implant procedure for stress incontinence. She suffered severe pain and an autoimmune reaction from the device that changed her life forever. After discovering at the time these devices could not be fully removed in Australia, Carolyn flew to the USA to have it removed. When she returned, she created a support group for women who are permanently injured by transvaginal mesh devices. The support group has helped many women understand that their symptoms are mesh related, because complications are not widely recognised by doctors and gynaecologists. Carolyn has written to senators, RANZCOG, the Therapeutic Goods Administration and media for over two years. This led her to Senator Derryn Hinch who took on her cause and secured a senate inquiry into transvaginal mesh. Carolyn’s ultimate goal is to have transvaginal mesh banned in Australia because the injuries can be catastrophic and many women will never recover.
Highly Commended is…
Petrina Lawrence
Petrina has been a consumer of the health system since being diagnosed as a child with Juvenile Rheumatoid Arthritis. Following this, she became the carer of her mother who was diagnosed at the age of 61 with early onset dementia. Driven by her experiences of accessing care, Petrina was motivated to create change and has been on various Health Network committees. More recently, Petrina has joined the Royal Perth Hospital (RPH) Consumer Advisory Council in 2012 where she took on the position of Chair.
Petrina is a highly respected in her role as Chair of the RPH CAC and works closely with RPH Director of Consumer Engagement Todd Gogol. In 2015 and with support from Todd, Petrina completely redeveloped the then existing CAC to embark on a new structure and format supported by The Consumer Engagement Strategy 2015-2017. Petrina led the recruitment of a new generation of CAC members that are current users of RPH services. Over 50 consumers have been recruited and not only sit on the CAC, but across working groups and other RPH committees.
Finalists are…
Kerry Donovan
Kerry Donovan has extensive experience in the training and workforce development sector where she spent the last fourteen years working for Challenger Institute of Technology at the senior and executive level. She is passionate about driving organisational and cultural change, transforming organisations to be more customer-focused, efficient and innovative.
Kerry has a special interest in the health sector gained through partnering with hospitals and aged care facilities to enhance training experiences for students. Since late 2014 Kerry has been a member of the Murdoch Consumer Consultative Committee.
Dorothy Harrison
Dorothy Harrison is the mother of two sons and grandmother of three, all born at Armadale Memorial Hospital. She has lived in Kelmscott since 1970 taking part in various school and youth groups along the way. Dorothy was appointed as a civil marriage celebrant in 1978. She has dealt with weddings, funerals and naming ceremonies ever since. This has given special insight into dealing with grieving families, and recent births, which are both relevant to hospital admissions. Dorothy has also survived two bouts of cancer and two total knee replacements so she knows a bit about being a patient.
Dorothy served five years with the Community Advisory Council at Armadale, completing courses in Cultural Diversity and Aboriginal traditions, policy writing, attending RCA investigations and assisting as national consumer with the Antimicrobial Standards through the Australian Commission on Safety and Quality in Healthcare.
Kim Hutchinson
Kim Hutchinson recently retired as a Police Inspector with West Australia Police after 44 plus years. He now resides in Maddington with his wife Maggie. In December 2014 Kim was diagnosed with Throat Cancer (he is a non-smoker) and underwent a treatment regime that included chemotherapy and radiation therapy. Cancer stopped Kim working for 12 months. Returning to duty in November 2015, he recognised the importance of demonstrating people can and do survive disease and continue to lead an effective and fulfilling life. After being diagnosed with cancer, the Cancer Council came into Kim and Maggies lives and became a great support for them. Promoting cancer awareness, support and positivity is now a continuing goal in Kim’s life. He involves himself (privately and publicly) whenever possible.

Janice Thair
Janice Thair moved from Karrinyup down to the Rockingham area in 1985. From 1989 – 1994 she instigated the formation of Rockingham Women’s Health now called South Coastal Women’s Health.
Janice was also on the Fremantle Hospital Board from 1994 to 1996 and in 2002, she became involved in lobbying to get the local hospital redeveloped (Rockingham General Hospital) and the joined the fledgling Community Advisory Council (CAC).
During this time, Janice set up the ‘Friends of the Hospital’. She is proud of the wonderful concierge service the volunteers still supply today, including the other great services the Friends of the Hospital render to the community.
Janice has been involved with the CAC for 15 years. She has seen the Rockingham District Hospital grow to the fantastic General Hospital it is today, Janice loves that she has been able to serve her community.














